Overhead athletes subject their shoulders to extreme repetitive torque, compression, distraction, and translation stresses, resulting in adaptive changes of the soft tissues and osseous structures within and around the glenohumeral joint. These anatomic adaptations result in biomechanical enhancements, which improve performance. Understanding the difference between necessary and adaptive changes and pathologic findings is critical when making treatment decisions. Injuries to the shoulder of the overhead athlete can be generally classified into three groups: internal impingement, internal impingement with acquired secondary anterior instability, and primary anterior or multidirectional instability. Although advances in surgical techniques have allowed surgeons to address the pathology in these groups, merely attempting to restore the shoulder to so-called normal can adversely alter adaptive changes that allow high levels of performance.
The glenohumeral joint of overhead athletes, especially pitchers, is subject to repetitive torque, compression, distraction, and translation. Over time, these stresses result in adaptive changes of the rotator cuff, capsulolabral complex, biceps tendon, and humeral head as well as other soft-tissue and osseous structures within and around the glenohumeral joint. A clear understanding of these adaptive changes is vital for appropriate diagnosis and management of sports-related injuries and associated pathology in this population. Familiarity with the anatomy of the thrower's shoulder and the contrast between pathoanatomy and adaptive changes that are critical for performance, along with careful evaluation of patient history, physical examination findings, and changes on MRI, can help the clinician manage expectations for return to play (RTP) and avoid overtreatment in overhead-throwing athletes.
Effective pitching requires the generation of high levels of arm speed. By creating greater momentum, pitchers can impart more energy to the ball. The best pitchers are able to generate considerable arm speed through adaptive changes, a greater total arc of motion, and specific throwing mechanics.[1–3] Through this process, tremendous stresses are placed on the shoulder. Effective peak angular velocities for internal rotation have averaged 6,180 degrees per second during acceleration.[4] As a result of this violent acceleration and hyperabduction, the rotator cuff, capsulolabral complex, biceps tendon, and glenohumeral ligaments are all susceptible to stretch, peel-back, and delamination injuries via compressive and shear forces.[5–12] In contrast, the larger muscles groups, such as the latissimus dorsi, are less commonly involved.
The general stages of throwing are the windup, early cocking, late cocking, acceleration, deceleration, and follow-through (Figure 1). The large muscle groups in the lower extremity, core, and upper extremity act as part of a kinetic chain that coordinates transmission of force from the legs and trunk to the upper extremity for ball release.[13] The transition between the late cocking phase and the acceleration phase is the critical point at which many injuries occur.
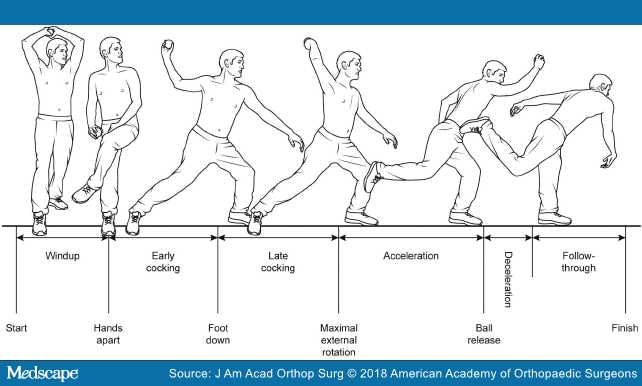
Figure 1.
Illustration showing the phases of throwing.
In late cocking, the shoulder is abducted, and the anterior capsule is under major strain as it attempts to restrain anterior translation of the humerus. Repetitive and excessive humeral external rotation by throwers may increase shoulder laxity.[14] Repetitive hard throwing is also thought to cause tensile failure and attenuation of the anterior capsule. Furthermore, stretching of the coracohumeral ligament may occur during forced external rotation in the overhead athlete.[8] With the arm in the 90°-90° position, the undersurface of the posterosuperior rotator cuff makes contact with the posterosuperior glenoid labrum and may become pinched between the labrum and the greater tuberosity, resulting in internal impingement.[11,12] In addition, shear forces increase at the biceps anchor and the posterosuperior labral attachment.[7]
The transition from the late-cocking to the acceleration phase involves coordination of eccentric and concentric muscle activities, which optimizes both performance and functional stability throughout the rapid range of motion. During the late cocking phase, the shoulder is abducted and externally rotated, which is accomplished by contraction of the posterior structures and both stretching of anterior static structures and eccentric firing of the anterior dynamic stabilizing structures. The infraspinatus and teres minor contract while the subscapularis, pectoralis major, and latissimus dorsi form an "anterior wall" that provides stability to the anterior aspect of the shoulder joint.[15] At this point, the supraspinatus is the least active of the rotator cuff muscles.
To transition from the late-cocking phase to the acceleration buildup, the eccentric and concentric balance must shift. The posterior deltoid keeps the arm abducted during shoulder internal rotation. The anterior cuff must then fire to internally rotate the shoulder and generate sufficient torque to impart substantial energy to the ball. In addition, the large anterior muscle groups, such as the pectoralis major and latissimus dorsi, act to internally rotate the shoulder with concentric contraction. The posterior rotator cuff (ie, the teres minor moreso than the infraspinatus) acts as a force couple to these anterior structures by eccentrically firing, which provides a posterior stabilizing force.[16]
During acceleration, professional throwers rely less on the rotator cuff and more on the pectoralis major, latissimus dorsi, triceps, and serratus anterior muscles.[17] In contrast, deceleration relies more on the rotator cuff, especially during follow-through, when the rotator cuff acts eccentrically and is subject to tensile stress. During follow-through, the posterior capsule and posterior cuff are subject to substantial eccentric stresses, which can be up to 108% (±16%) of body weight.[6] Repetitive stress on the posterior cuff may lead to muscular fatigue, which can increase transfer of stress to the posterior capsule.[9]Chronic microtrauma and tearing of the posterior capsule may precipitate a fibroblastic healing response, increased collagen deposition, and loss of tissue compliance, resulting in a stiff posterior cuff and capsule.[10]
The shoulder joint is stabilized by both static and dynamic structures. The static stabilizers include the glenohumeral joint geometry, the glenohumeral ligaments, and the capsulolabral complex, which act via joint conformity as well as adhesion-cohesion. These stabilizers are subject to mechanical failure.
The most important dynamic stabilizers are the rotator cuff and the long head of the biceps. The long head of the biceps tendon acts as a dynamic stabilizer in the abducted and externally rotated position.[15,18] These structures also actively stabilize the glenohumeral joint via concentric and eccentric muscle contraction forces and are subject to fatigue as well as overt mechanical failure.
Injury to the thrower's shoulder is often acute on chronic, with overuse and fatigue as important factors. When the kinetic chain is evaluated, scapular dysfunction and rotator cuff imbalance may be present. As noted previously, the thrower's shoulder may develop an excessively tight posterior capsule, resulting in a glenohumeral internal rotation deficit (GIRD) that leads to internal impingement with or without secondary instability. Primary or multidirectional instability may also be present.
When evaluating the thrower's shoulder for pathoanatomy, the clinician must understand the coexistence of adaptive anatomic and nonpathologic changes that are the result of repetitive stresses associated with throwing (Table 1). As a result of these changes, a high percentage of throwing athletes demonstrate asymptomatic but abnormal findings on MRI.
Lesniak et al[19] evaluated the MRI results of 21 asymptomatic professional pitchers and found that 52% had rotator cuff tears (RCTs), 48% had superior labrum anterior to posterior (SLAP) tears, and 62% had anterior or posterior labral tears. These findings correlated with the number of career innings pitched. In another MRI study of asymptomatic professional baseball pitchers, Miniaci et al[20] found that 79% of shoulders had labral pathology, with no statistically significant difference between the dominant and nondominant shoulders. In a prospective cohort study, Connor et al[21] evaluated MRI shoulder scans of asymptomatic elite overhead athletes and found that although their nondominant rotator cuffs were normal, 40% of the dominant shoulders exhibited findings consistent with partial- or full-thickness RCTs. Despite these findings, none of the athletes reported any shoulder problems during the 5 years after the MRIs were obtained.
The proximal humerus is retroverted in utero (mean, 78°) and derotates over time.[22] It reaches a mean of 65° from 4 months to 4 years of age and is approximately 38° in children 10 to 12 years of age.[22] The most rapid changes occur before age 8 (± 2.12) years and continue until the appearance of the radial groove (approximately age 16 years).[22] In the average adult, mean retroversion differs between 33° in the dominant arm and 29° in the nondominant arm. No substantial differences between sexes were observed in a study of retroversion of the humeral head.[23]
In contrast, further increased humeral retroversion is found in the thrower's dominant shoulder. These bony adaptations contribute to the rotational changes found in these shoulders.[24] These adaptive and often asymptomatic physeal changes occur throughout adolescence and have been observed in the dominant throwing arms of skeletally immature baseball players.[25] It has been proposed that these adaptive bony changes are the result of derotation restriction rather than an active increase of retroversion from throwing[26] (Figure 2).
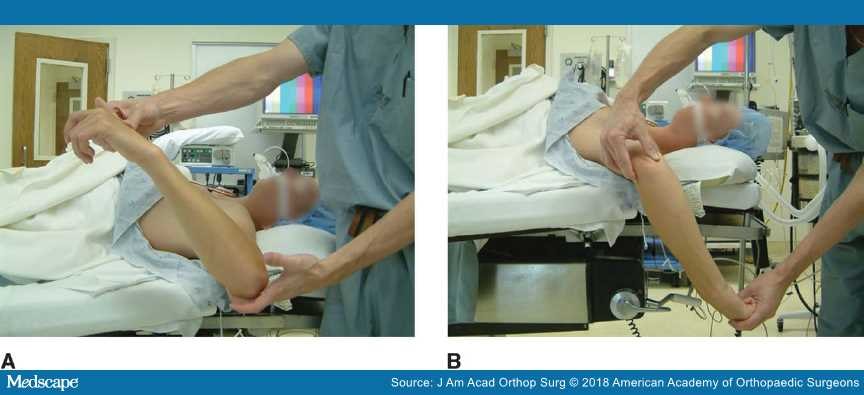
Photographs showing decreased internal rotation (A) and increased external rotation (B) in a thrower's shoulder. (Courtesy of Mark Schickendantz, MD, Cleveland, OH.)
Collegiate throwers have an increased average retroversion of 36.6° (±9.8°) and a total arc of motion of 159.5° in the dominant arm versus a decreased average retroversion of 26° (±9.4°) and total arc of motion of 157.8° in the nondominant arm.[27] Collegiate pitchers had increased dominant arm external rotation when measured at zero and 90° of abduction, which was associated with greater humeral retroversion.[28] Similarly, professional baseball pitchers' dominant shoulders showed increased external rotation and humeral/glenoid retroversion.[29] These adaptive changes are thought to pre-position the throwing arm in external rotation, leading to less anterior shoulder strain and imparting greater kinetic energy via increased rotational torque while throwing.
In addition to enhancing performance, adaptive changes to the shoulder may decrease injury rates. In one recent study, a correlation was found among injured professional pitchers with more missed playing days and a lower degree of retroversion shoulder dominance.[30]
To help guide treatment, injuries related to the thrower's shoulder can be generally classified into three groups. Group 1 injuries are caused by internal impingement. Group 2 injuries are caused by internal impingement with acquired secondary anterior instability. Group 3 injuries are the result of primary anterior or multidirectional instability. Within each group, athletes exhibit specific clinical histories, physical examination findings, and MRI changes.
During the late-cocking phase, the arm is positioned in abduction and extreme external rotation. In this position, there is mechanical pinching of the posterolateral rotator cuff and the labrum between the posterolateral portion of the greater tuberosity and the posterosuperior glenoid (Figure 3). Although such pinching can be seen as part of a normal biomechanical process in high-level throwers, repeated mechanical impingement can lead to shoulder pathology. The thrower will experience posterior pain during late cocking. This pain is mechanical and positional in nature; it hurts each time the athlete moves the shoulder into the externally rotated/abducted position achieved during the late-cocking phase of the throwing motion. In addition, the athlete may have posterolateral cuff pain. On physical examination, a positive internal impingement sign of deep posterior shoulder pain is exhibited when the arm is brought into a position similar to the late-cocking phase of throwing, that is, abduction of 90° to 110°, extension of 10° to 15°, and maximal external rotation.[31] MRI findings that coincide with this posterolateral impingement include rotator cuff injury at the junction of the supraspinatus and infraspinatus, posterosuperior labral injury, and cystic changes in the posterolateral tuberosity (Figure 4).
Arthroscopic image of a shoulder demonstrating internal impingement of the posterolateral rotator cuff and the labrum in the lateral decubitus position. B = biceps tendon, G = glenoid, H = humeral head, SS = supraspinatus. (Courtesy of Mark Schickendantz, MD, Cleveland, OH.)
Axial T2-weighted MRI of the glenohumeral joint showing changes commonly found in throwers, including posterior capsule thickening and posterior cuff changes (A) and posterolateral glenoid cystic changes (B). (Courtesy of Mark Schickendantz, MD, Cleveland, OH.)
A so-called peel-back lesion of the biceps anchor and labrum occurs during abduction-external rotation (ABER) as the biceps tendon moves posterior to the joint behind the tuberosity and pulls on the labrum.[32] The fibers of the biceps tendon are oriented to resist traction. However, the strain pattern of the ABER position does not coincide with direct traction; instead, it causes a torsional strain that can lead to failure at the biceps anchor, resulting in a SLAP lesion. In the thrower, the SLAP lesion reveals a demonstrable peel-back sign extending posteriorly. The typical thrower's SLAP lesion does not extend anteriorly[33](Figure 5).
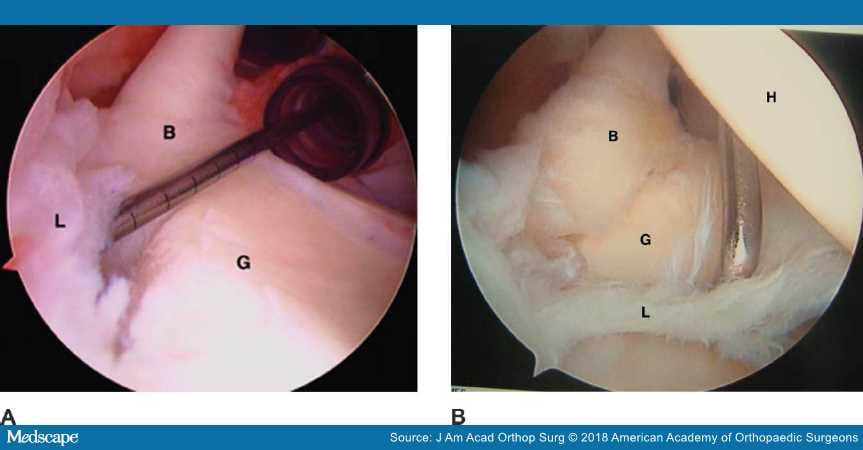
Figure 5.
Arthroscopic images of a thrower's shoulder demonstrating type I (A) and type III (B) superior labrum anterior to posterior lesions. B = biceps tendon, G = glenoid, H = humeral head, L = labrum. (Courtesy of Mark Schickendantz, MD, Cleveland, OH.)
During the follow-through phase of throwing, repetitive loads to the posteroinferior capsule can lead to contracture of the posterior band of the inferior glenohumeral ligament (PIGHL).[7] After ball release, the arm moves ahead of the body and exerts a large distraction force of approximately 750 N (80% of body weight),[34] which acts on the posteroinferior capsule. A tight posterior capsular contracture has been shown to shift the glenohumeral rotation point in a posterior and superior direction.[35] As an adaptive response, it allows more clearance of the greater tuberosity over the glenoid rim during ABER; therefore, the athlete can hyperexternally rotate the shoulder.
A tight PIGHL can also lead to anterior pseudolaxity. The humeral head acts as a cam to tighten the anterior structures, but as the tight PIGHL shifts the center of rotation posteriorly and superiorly, the cam effect of the head is lost anteriorly. It is important to recognize that this apparent anterior pseudolaxity without subluxation is not the source of pathology, especially in the presence of a posterior SLAP tear.
Like all adaptive responses, too much compensation along the spectrum can lead to pathology. Although it was previously noted that pitchers gain increased external rotation and lose internal rotation, this should not come at the expense of total arc of motion. Thickening and contracture of the PIGHL can lead to GIRD. With a loss of ≥25° of total arc of motion, GIRD is symptomatic.[7] In the ABER position of late cocking, the posterior band of the IGHL is bowstrung beneath the humeral head. The biceps vector shifts posteriorly and twists at its base, maximizing peel-back forces. As a result of the tight posteroinferior capsule, a pitcher may show poor pitching mechanics and a breakdown in the kinetic chain. These breakdowns can include hyperexternal rotation, hyperhorizontal abduction (out of the scapular plane), a dropped elbow, and premature trunk rotation.[7] In fact, pitchers with GIRD are nearly twice as likely as pitchers without GIRD to be injured.[36]
As part of the internal impingement spectrum, the rotator cuff may be injured. During the late-cocking phase, the rotator cuff is twisted like a rope. During follow-through, the rotator cuff fibers are then placed under stretch or eccentric loading, resulting in further tensile stress. This repetitive twisting and pulling can result in tendon failure. In this case, overhead throwers may also experience anterolateral pain that is aggravated by overhead activities. They may experience more pain during the acceleration and follow-through phases. The pitcher may take longer to warm up. Once warmed up, the pitcher may feel okay; however, the pain may return later in the game.
The spectrum of rotator cuff injuries ranges from tendinitis and tendinosis to partial-thickness tears. Partial-thickness tears tend to be articular sided and most often occur at the junction of the supraspinatus and infraspinatus tendons (Figure 6). The acronyms PASTA (ie, partial articular supraspinatus tendon avulsion) and PAINT (ie, partial articular tear with intratendinous extension) are often used to describe these lesions.[37,38] Full-thickness tears are rare in the overhead athlete.[39]
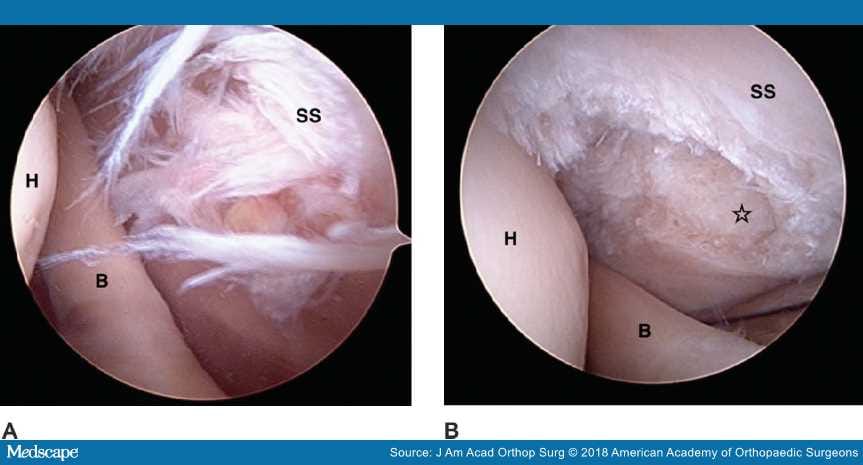
Figure 6.
Arthroscopic images of a shoulder demonstrating partial-thickness (50%) rotator cuff tear before (A) and after (B) débridement. The star indicates an area of partial tear débridement. B = biceps tendon, H = humeral head, SS = supraspinatus. (Courtesy of Mark Schickendantz, MD, Cleveland, OH.)
As mentioned previously, increased external rotation is an adaptive change that allows overhead athletes to improve their performance. However, some authors have speculated that this increase in external rotation can lead to repetitive microtrauma in the anterior structures, resulting in stretching of the anterior IGHL and anterior capsule. Excessive repetitive hyperexternal rotation and hyperhorizontal abduction and subsequent anterior stretching can lead to symptomatic anterior instability.[12,40]A cadaver study showed that increasing anterior capsular laxity could exacerbate internal impingement during the late-cocking phase of the throwing motion.[14]
In athletes with a group 2 injury, a deep anterior pain is experienced during the late-cocking and acceleration phases. Because of increased anterior translation and associated anterior instability, anterior labrum tears with or without an associated internal impingement type posterior-superior SLAP tear may develop in these athletes. Although most overhead athletes demonstrate 1+ passive anterior translation on physical examination (ie, increased anterior translation of the humeral head without subluxation) caused by adaptive changes, 2+ anterior translation (ie, translation with subluxation of the glenohumeral joint) should be considered pathologic.[39]Patients with group 2 injuries (ie, injuries caused by internal impingement with acquired secondary anterior instability) may experience tensile failure of the anterior supraspinatus (ie, PASTA lesions). In addition, anterior subluxation can lead to scuffing of the anteroinferior labrum or, in extreme cases, a Hill-Sachs impression lesion.
As in any athlete with shoulder pain, primary or multiplane instability can be the source of pathology. Throwers with group 3 injuries experience extremity fatigue or describe a so-called dead arm. They may have nonspecific pain at the rotator cuff. Overhead athletes rely on the rotator cuff to keep the glenohumeral joint stable during the throwing motion; as the cuff fatigues, subluxation episodes may occur. When these athletes play, they start the game slowly but improve in the middle innings as the rotator cuff warms up. However, as the game progresses and the rotator cuff begins to fatigue, symptoms worsen. In these athletes, physical examination findings, such as the sulcus sign and positive apprehension and relocation tests, are consistent with primary anterior or multidirectional instability. Positive MRI findings are often minimal.
Overhead athletes require coordination of the kinetic chain to deliver energy from the legs and the core through the arm to a ball, racket, or other object. A break anywhere along the chain can predispose an athlete to injury. It is important to identify players at risk for injury, especially in the off-season, preseason, or at baseball spring training. During the entrance or preseason physical examination, the total arc of motion should be measured on both sides and compared. A major loss of motion from GIRD found on physical examination should be documented, and the thrower should begin a posterior capsular stretching program.
Ninety percent of throwers respond to a nonsurgical stretching program, such as the sleeper stretch exercise.[7]Wilk et al[36] observed that pitchers with insufficient external rotation in the throwing shoulder (ie, <5° greater external rotation on the throwing side) were 2.2 times more likely to be placed on the disabled list because of a shoulder injury and 4.0 times more likely to require shoulder surgery than pitchers who exhibited increased external rotation on the throwing side. A specific subset of overhead athletes may develop the SICK scapula syndrome (ie, scapular malposition, inferior medial border prominence, coracoid pain, and dyskinesia of scapular movement).[41] These patients will present with an asymmetric "dropped scapula" on physical examination, which not only can lead to fatigue of the scapular musculature but also can decrease shoulder internal rotation.
In addition to maintaining range of motion and avoiding excessive stretching of the anterior capsule, overhead athletes need to maintain balanced rotator cuff strength and scapular control. Professional baseball pitchers tend to have greater internal rotation strength than external rotation strength in the dominant arms. Wilk et al[42]analyzed the isokinetic muscular performance characteristics of the external/internal rotator muscles of professional baseball pitchers and noted that torque testing showed approximately 5.5% less external rotation strength at lower speeds (180 deg/sec) for the throwing shoulder, but this side-to-side muscular imbalance appears to even out at higher speeds (300 deg/sec). This same study suggested that for appropriate glenohumeral muscle balance in asymptomatic throwing shoulders, external rotation should be ≥65% of the strength of internal rotation.[42] In a separate study, preseason weakness of external rotation and supraspinatus strength was associated with in-season throwing-related injuries requiring surgical intervention.[43] Throwers should also have increased shoulder adductor strength, which is important in the late-cocking and acceleration stages.[44]
A level IV case series showed that 10 of 15 overhead-throwing athletes treated with a nonsurgical regimen for a type II SLAP tear returned to play at the same or higher level of performance than before the injury. The patients required a mean of 18 physical therapy sessions (range, 4 to 40 visits) before returning to sport.[45]
A retrospective review of a single Major League Baseball organization by Fedoriw et al[46] evaluated surgical versus nonsurgical treatment of type II or type II posterior-variant SLAP tears. Twenty-one pitchers with these tears completed a nonsurgical algorithm focusing on the correction of scapular dyskinesia, posterior capsular contracture with glenohumeral internal rotation deficit, and concomitant lapses in the overall kinetic chain. Two rounds of physical therapy were attempted: the first with the team trainer in the player's respective city and the second after having visited the study authors. This was then followed by a graduated return to a 6-week pain-free throwing program. The RTP rate was 40%, and the return to prior performance (RPP) rate was 22%.
Fedoriw et al[46] noted that Thus, it appears that for pitchers, nonsurgical treatment of type II SLAP tears may have a more successful outcome than surgical intervention.
"the RTP rate for 27 pitchers who underwent surgical procedures was similar at 48%, and the RPP rate was lower at 7%. For 10 position players treated nonsurgically, the RTP rate was 39% and the RPP rate was 26%. The RTP rate for 13 position players who underwent 15 procedures was higher at 85%, with a higher RPP rate of 54%."
Group 1 injuries are related to internal impingement, which can lead to labral and rotator cuff injuries. When patients with group 1 injuries are evaluated, it is extremely important to understand that their shoulders have adaptive changes that allow them to perform at a high level. Merely attempting to restore their shoulders to normal without taking into consideration these adaptive changes will prevent these athletes from returning to preinjury form. One of these adaptive changes is anterior capsulolabral pseudolaxity, which allows for increased external rotation and abduction. Thus, when a SLAP lesion is repaired in an overhead athlete, the surgeon should focus more on managing the posterior SLAP tear (if present) and be wary of placing anchors anterior to the biceps because this will tighten the shoulder anteriorly and reduce the hyperexternal rotation available to the athlete.
Although type I SLAP tears typically can be débrided successfully, the outcomes of type II SLAP repairs are more unpredictable in the overhead athlete. Low-level evidence has shown that it takes 11 to 12 months for RTP after a type II SLAP repair in the overhead athlete.[47,48] A case series of arthroscopic repairs of type II SLAP tears in overhead athletes showed that although a 93.3% satisfaction rate was achieved with the repairs, the athletes believed they had reached only a mean rate of 84.1% of their preinjury performance level.[47] A systematic review of type II SLAP lesion repairs with a 2-year follow-up showed that for all athletes studied, only 73% returned to their previous level of play; for overhead athletes, even fewer returned to their previous level of play (63%).[49]
When an RCT is encountered, the surgeon is often faced with the dilemma of débriding or repairing it. In the experience of the senior author (M.S.S.), an RCT in an overhead athlete is a relatively shallow, partial articular lesion (<50% thickness). In this case, it is typically better to simply débride the partial tear rather than attempt to repair it.
Most rotator cuff lesions are ulcerative lesions with an associated delamination, making anatomic repair extremely difficult if not impossible. In a retrospective study of 82 professional pitchers with small partial-thickness RCTs treated with surgical débridement, Reynolds et al[50]reported that, of 67 pitchers with RTP data, 76% were able to return to competitive pitching at the professional level, although only 55% achieved RTP at the same or higher performance level. This is in contrast to a markedly lower performance level for pitchers with full-thickness tears. Mazoué and Andrews[51] evaluated a series of 12 professional pitchers with full-thickness RCTs treated with mini-open repair and found that only 1 pitcher was able to return to a high competitive level. The remaining patients either never returned or pitched a half season or less.
Low-level evidence is available for concomitant SLAP and rotator cuff repairs, specifically in overhead athletes with GIRD. In a series of 17 overhead athletes with GIRD who underwent SLAP repair combined with repair of the infraspinatus, Van Kleunen et al[52] reported that only 6 patients (35%) returned to preinjury or higher levels of performance. Six players were unable to return to play (35%) and five of the 17 patients studied (29%) returned to play at a lower level, "either playing the same position or else forced to switch to another position of play because of a decline in throwing velocity." The authors concluded that these patients were unlikely to return to their preinjury level of play.[52]
A level III study of 23 collegiate or professional overhead athletes revealed that at least 1 year (mean, 3 years) after type II SLAP lesion repairs, only 57% returned to preinjury level of competition despite high American Shoulder and Elbow Surgeons scores.[53] The athletes' RTP correlated with the presence of a partial-thickness RCT. The same study indicated that for the evaluation of the overhead athlete, the Kerlan-Jobe Orthopaedic Clinic shoulder and elbow score was a more accurate assessment tool than the American Shoulder and Elbow Surgeons score.[53]
The second group of injuries involves internal impingement with acquired secondary anterior instability. For patients with group 2 injuries, the same principles apply regarding débridement versus repair of either a SLAP tear or RCT. In addition, the secondary instability should be addressed, and anterior labrum tears should be repaired as indicated. When the surgeon notes a persistent drive-through sign after repair of the SLAP lesion, plication of the anterior band of the IGHL may be considered. Plication of the area of the anterior capsule that appears most attenuated, including ≥20% of the anterior capsule within the plication, is recommended.[54]
Few data are available on outcomes in patients with group 2 injuries, and RTP is less predictable in these patients than in patients with group 1 injuries. The only level II comparative study to analyze concomitant SLAP and Bankart repairs versus Bankart repairs alone found that patients with combined lesions did not have any more failures after surgery than did patients with an isolated Bankart lesion.[55]
Treatment of the overhead athlete with symptomatic primary or multidirectional instability is challenging. Before surgery is considered, the athlete needs to keep the rotator cuff strong and balanced and follow a scapular strengthening and maintenance program. Throwing volume should be monitored in these athletes because they tend to break down and experience pain after their cuff fatigues.
Should an exhaustive course of therapy be unsuccessful, surgical management in the form of a capsular shift may be considered. The capsular shift can be accomplished using sutures with or without anchors and either plicating the capsule to itself or to the labrum. Anterior, inferior, and posterior planes of laxity must be addressed. This is accomplished with a so-called 270° repair involving the rotator interval and the anterior and posterior bands of the inferior glenohumeral ligament.
The RTP rate in patients with group 3 injuries is highly unpredictable, and plication of the anterior capsule may restrict the athlete's necessary external rotation. As with group 2 injuries, evidence on outcomes is limited; however, a level III cohort study with a mean follow-up of 3.3 years following arthroscopic pancapsular suture anchor plication showed that 23 of 30 patients (76.7%) had returned to sport at or near their preinjury level.[56] The authors of the study also noted that there was a substantial difference in RTP in patients with traumatic versus atraumatic onset of symptoms (83% versus 44%, respectively).
Overhead athletes have adaptive structural changes to the shoulder that allow them to play at a high level. These adaptive changes do not necessarily represent pathology, and merely attempting to restore the overhead athlete's shoulder to normal may reverse these adaptations and prevent a return to the previous level of performance. It is easy to overtreat these athletes, and surgical outcomes may not be better—and may even be worse—than nonsurgical outcomes.

C/ San Pedro de Mezonzo nº 39-41
15701 – Santiago de Compostela
Teléfono: +34 986 417 374
Email: secretaria@sogacot.org
Coordinador del Portal y Responsable de Contenidos: Dr. Alejandro González- Carreró Sixto