Since bundled payment programs often include the reimbursement for complication and readmission, it has become increasingly important to identify patients at risk for perioperative complications [1, 2, 3, 4].
Being able to identify patients at risk for medical and surgical complications helps to better prepare the patient for the procedure based on patient-specific risk factors and invasiveness of the procedure and ultimately might help to reduce the overall complication rate. In the past, several significant risk factors for medical complications in spine surgery were identified utilizing multivariate analysis [5, 6, 7]. However, a risk stratification tool that is easy to integrate into clinical practice has been missing.
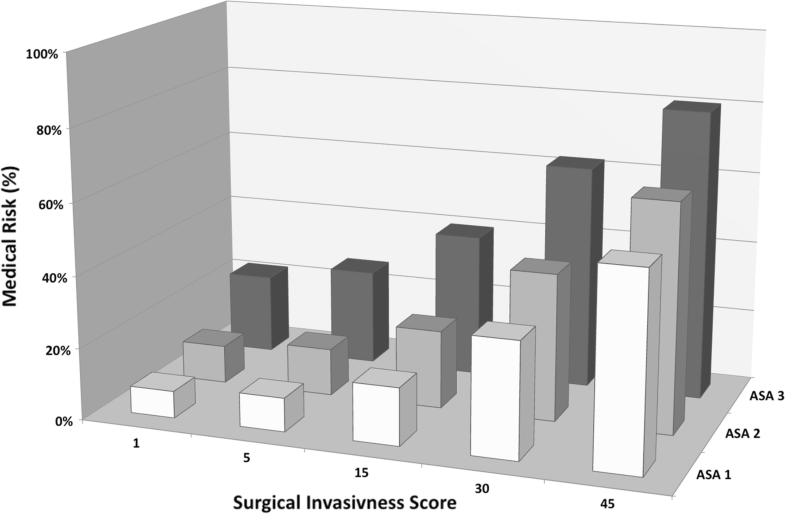
Lee et al. [8] created a validated model for predicting medical complications after spine surgery based on a prospective spine surgery registry. It is meant to simplify preoperative assessment by taking into consideration patient-specific risk factors as well as the invasiveness of the procedure (Fig. 1).
Fig. 1
The 3D model is showing that risk depends on two factors: patients’ comorbidity profile and invasiveness of surgery. Risk increases either through an increased amount of preexisting medical conditions or due to more invasiveness surgery. SpineSage™ is the first predictive model that connects either factors and predicts an individual patient risk
This risk calculator is available online free of charge. It allows the surgeon to calculate the risk for perioperative medical complication for a specific patient and procedure [8]. There are currently no data available that analyze the clinical value of this perioperative risk calculator.
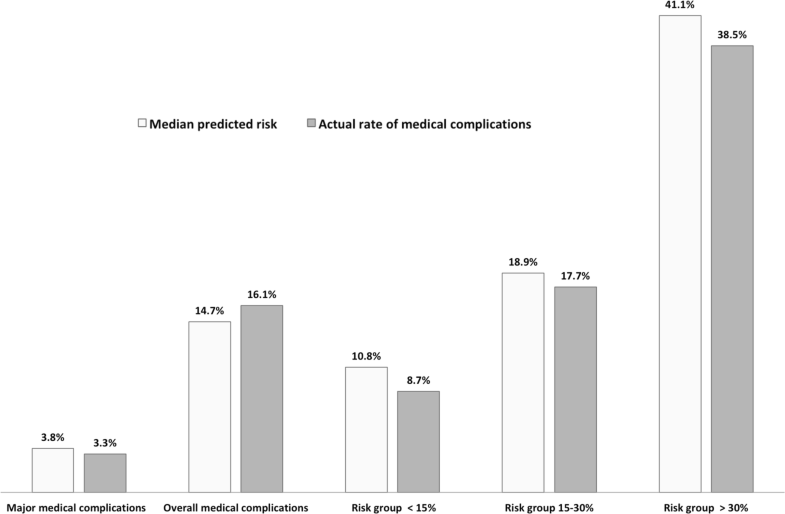
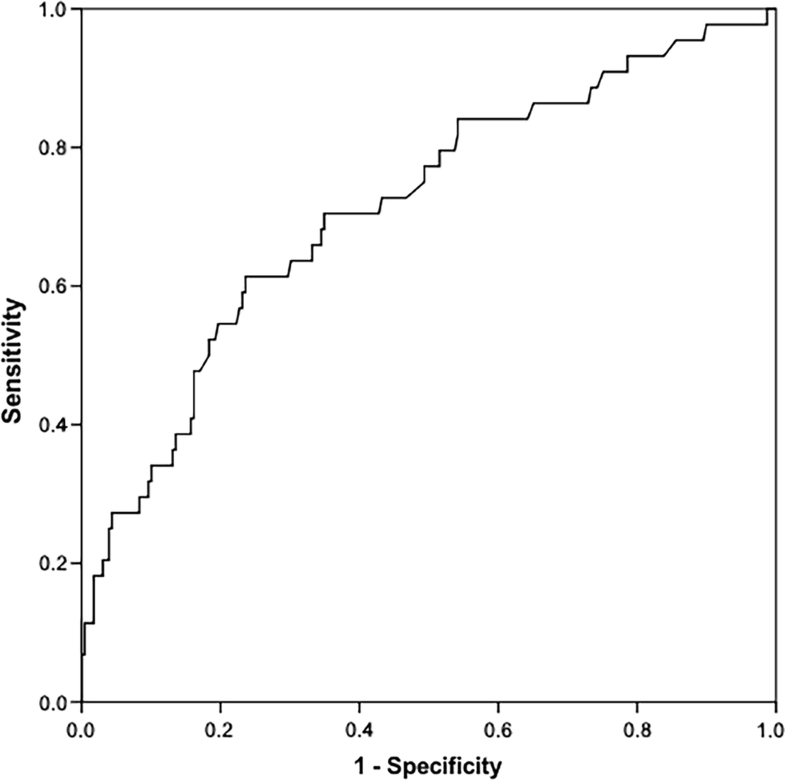
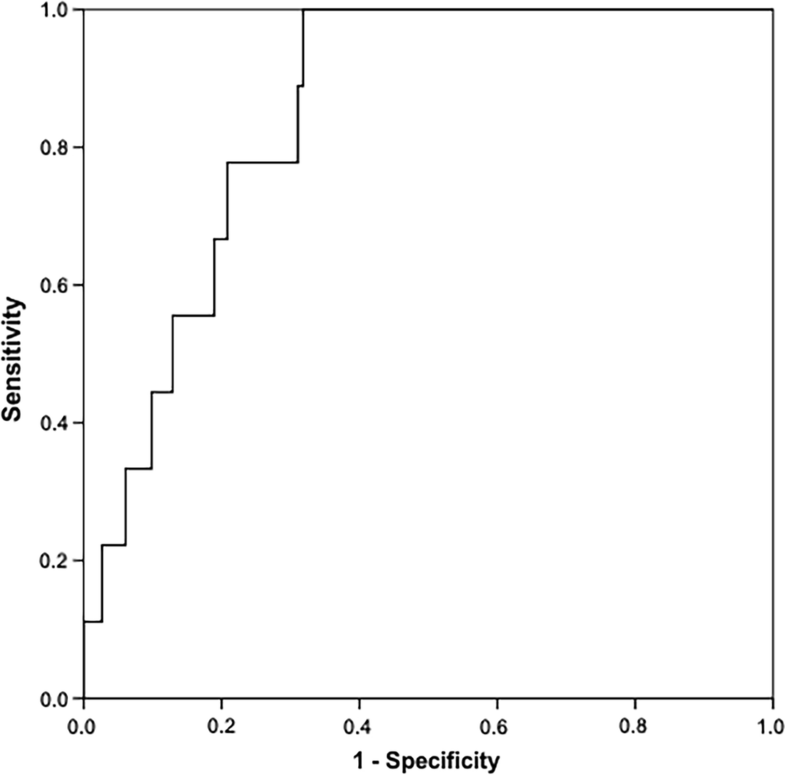
The current study reports the initial clinical experience with this risk assessment tool and analyzes the following research questions: (1) Is there a difference between the predicted overall medical complication rate and the observed complication rate? (2) What is the value of the tool for patients with different risk levels? (3) Furthermore, does the tool have a diagnostic value for the prediction of complication?