This article provides an overview of the methodology and characteristics of the expert participants of the Global Spine Care Initiative (GSCI) and describes of the expertise, clinical experience, and potential biases and conflicts of interests for each member of the GSCI Task Force.
World Spine Care was established in 2008, and its mission is to improve lives in underserved communities through sustainable, integrated, evidence-based spine care. To fulfill this mission, the World Spine Care leaders wished to develop an evidence-based model of care that could be integrated into healthcare programs and implemented anywhere in the world. Therefore, World Spine Care convened the GSCI to develop such a model.
Funding was provided by the Skoll Foundation that provided a matching grant. To receive the grant, GSCI members participated without any remuneration beyond travel expenses, which satisfied part of the requirement for the matching grant. The NCMIC Foundation provided funding to complete the matching requirement. The University of Ontario Institute of Technology-Canadian Memorial Chiropractic College Centre for the Study of Disability Prevention and Rehabilitation received a contract from the GSCI to provide a research librarian and project coordinator as well as first-level reviews of the literature for a number of the scientific papers that make up the proceedings of the GSCI.
The principal investigator (SH) invited co-investigators to form an executive committee. The primary requirement for the executive committee was extensive experience and qualifications in developing evidence-based guidelines and practice parameters for the management of spinal disorders and participation on the executive committee of prior task forces that addressed the management of spine-related complaints. Additional criteria for selecting executive committee members included: primary research or clinical career in spine care; knowledge of current evidence related to spine care; willingness to commit to the GSCI project over a period of 3 years without personal compensation; and no association with any commercial agency or industry that had financial interests in low- or middle-income countries.
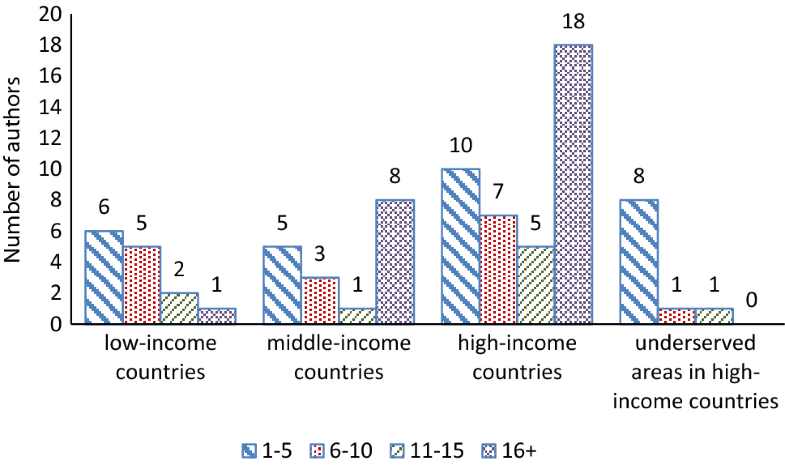
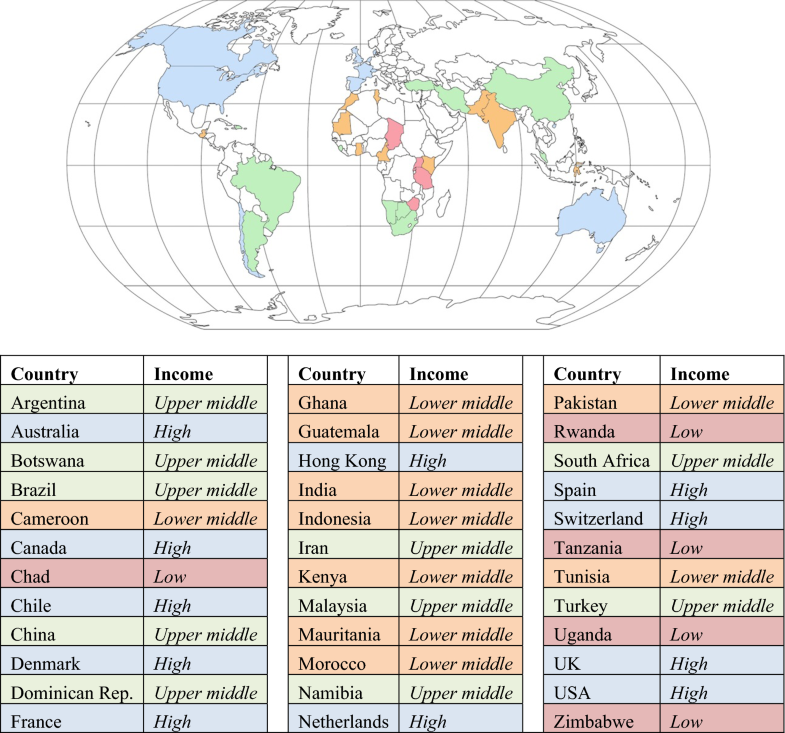
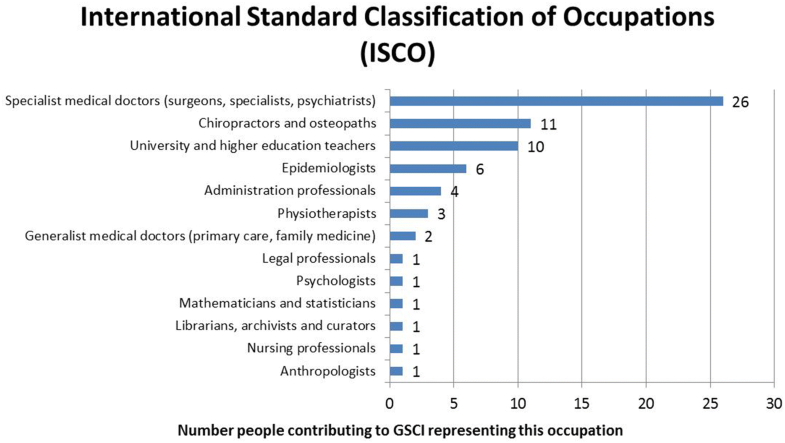
Once the executive committee was selected (RC, MN, PC, EH), they developed a list of additional experts to participate in the development of the GSCI articles and consensus process. The executive committee identified clinicians and scientists from around the world with primary interests and experience in spine care. Special effort was made to identify participants from low- and middle-income countries. However, finding these individuals was challenging since those who have an interest or expertise in spinal disorders and are willing to participate without compensation are rare. Healthcare resources tend to focus on infectious and general health issues, and spinal disorders tend to have very little priority in these countries. The executive committee was pleased to find some participants from low- and middle-income countries and other participants who provided health care in these regions. Participants were invited for geographic, professional, and scientific representation. All participants of the GSCI Task Force were invited to contribute to the GSCI model of care through a modified Delphi consensus process.
A series of meetings were convened in the first year to frame the scope of the project. The first meeting held in Chicago, Illinois (July 2014), outlined the core topic areas. The activities included describing the current global burden of spinal disorders through a comprehensive review of the literature for all types of communities and one to focus on the burden experienced by small communities and individuals since this has often been overlooked. Literature reviews were assigned to identify best practices that could be implemented within a spine care pathway, which included assessments, prevention, and treatments.
A meeting in Toronto, Canada (November 2014), and one in San Jose, California (March 2015), brought team members together to discuss their findings. After the third meeting, the topics and goals for the papers were finalized and the lead authors were designated to conduct their literature reviews and write their articles. After the first set of review papers were completed, additional lead authors drafted an evidence-based model of care based on the findings of the literature reviews and completed consensus processes.
Electronic surveys were delivered to each participant using Survey Monkey (SurveyMonkey Inc., San Mateo, California, USA) to collect competing interest and participant information. Surveys included rating scales, multiple-choice, and open-ended questions to allow the participant to include necessary demographic information (see Online Resource for the survey in Appendix 1). All participants were asked to provide consent to participate to allow their names to be listed as authors on the papers that they contributed to.
The questionnaire included:
- 1.
Information based upon the International Council of Medical Journal Editors conflict of interest form [6].
- 2.
Information based upon European Spine Journal requirements for reporting funding, bias, conflict of interest, or contributorship.
- 3.
Demographic and descriptive information about each participant (e.g., degrees, training, discipline, experiences relevant to the project).
- 4.
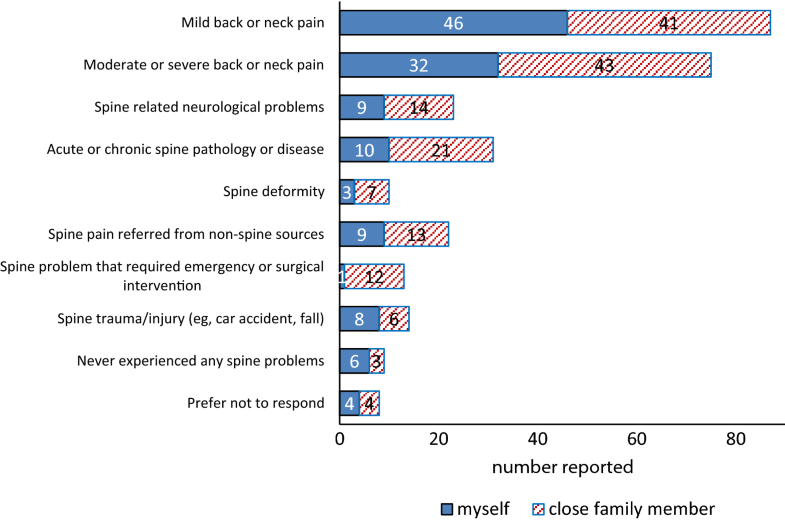
Experience with spinal conditions personally or by a family member.
The National University of Health Sciences Institutional Review Board approved this study (#H-1503). All authors were informed and provided their consent to participate.