Mohamed A. Abdel Salam, MD; Mohammed M. Mansour, MD; Ahmed El Naggar, MD
Curr Orthop Pract. 2018;29(4):337-342.
Background: Chronic recalcitrant heel pain is a commonly observed painful condition that often frustrates both the patient and the treating physician.
Methods: Twenty-four patients (14 men and 10 women) with chronic resistant heel pain were included in this study. All patients were locally injected by platelet rich plasma (PRP), and according to the results of injection, patients were divided into two groups: group A patients had significant improvement and group B had no specific progress. Group B patients underwent surgical decompression of the first branch of lateral planter nerve "Baxter's nerve" with release of medial planter fascia and calcaneal drilling.
Results: PRP injection showed 58.3% satisfactory results with improvement of the Plantar Fasciitis Pain/Disability Scale (PFPS) from 79.15 (range, 71.8 to 83.8) to 22.3 (range, 15.4 to 25.5) and improvement of the Foot Function Index (FFI) from 160.42 (range, 155 to 166) to 30.4 (range, 23 to 38). PRP injection failed to provide satisfactory results in 10 patients (41.7%). This group of patients showed 90% satisfactory outcome after surgical interference with improvement of the PFPS from 60.8 (range, 55.4 to 63.8) to 21.8 (range, 16.4 to 25.6) and improvement of the FFI from 143.4 (range, 122 to 155) to 38 (range, 31 to 52).
Conclusions: Conservative methods can provide satisfactory outcome in up to 90% in the treatment of chronic heel pain. Resistant cases can be managed by a local injection of PRP; surgical management should be reserved for patients who do not respond to PRP injection. Surgical management requires release of Baxter's nerve and medial planter fascia, and calcaneal drilling.
Heel pain is a common presenting symptom in orthopaedic practice and has a wide variety of causes, including plantar fasciitis, fat pad atrophy, calcaneal stress fracture, neoplasm, and infection. Entrapment of the first branch of lateral planter nerve, "Baxter's nerve," accounts for about 20% to 30% of heel pain and produces symptoms that are indistinguishable from plantar fasciitis. Although conservative management of heel pain has a success rate reaching 80% to 90%, chronic persistent heel pain remains a challenge to manage.[1]
Protein rich plasma (PRP) injection provides high success rates that can reach 60% to 80% for treatment of chronic heel pain after failure of noninvasive conservative methods, and it is safe to use with no risk of fat pad atrophy or plantar fascia rupture both of which have been reported with corticosteroid injection.[2] If surgery is indicated, release of all possible causes of Baxter's nerve entrapment with calcaneal drilling improves the surgical outcome and patient satisfaction.
The purpose of this study was to suggest a treatment algorithm for chronic resistant heel pain.
Our local ethical review board approved this study. In the period from January 2013 to March 2015, 24 patients (14 men and 10 women) with chronic resistant heel pain were included in the study. Average patient age was 41.9 yr, ranging from 33 to 54 yr. All patients complained of chronic heel pain mostly on the medial side of the heel, which characteristically increased in the early morning. The duration of symptoms was 13.7 mo, ranging from 8 to 24 mo.
Inclusion criteria were age more than 18 yr; duration of symptoms longer than 6 mo; failed trials of conservative treatment, including stretching exercises, nonsteroidal anti-inflammatory medication, and local corticosteroid injections; and a visual analog scale for pain of more than 5 during the first steps in the morning. Exclusion criteria were local injection within 6 mo prior to study, previous surgery for plantar fasciitis, diabetic peripheral neuropathy or vascular insufficiency, and pregnancy. Since the site of pain is a very important sign to confirm a diagnosis of plantar fasciitis, any patient who did not have pain localized to the medial side of the heel in relation to the medial tubercle of the calcaneus and origin of the medial plantar fascia was excluded from the study.
All patients were instructed to stop any physical therapy for chronic heel pain for 6 wk and any nonsteroidal anti-inflammatory medication the week prior to the PRP injection. All patients underwent a thorough physical examination of the foot and ankle, including stance, gait, and ankle range of motion, noting any restriction of ankle dorsiflexion. Also any abnormality in neurological or vascular evaluation was recorded.
Plain radiographs of the ankle and foot were obtained to rule out any other causes of heel pain. A calcaneal spur was found in 21 patients, with an average length of 2.25 mm (1-5 mm), but there was no relationship between the length of the spur and the severity of pain.
Patients were evaluated using the Plantar Fasciitis Pain Disability Score (PFPS) and Foot Function Index (FFI). The average pre-study PFPS was 79.6 points (71.8 to 83.8 points), while the average FFI was 163.8 points (155 to 179 points).
All patients were injected with PRP and were then classified at 3 mo into group A and group B according to their response to PRP injection (group A, significant improvement of symptoms after injection; group B, poor improvement of symptoms). Group B patients proceeded to surgical intervention.
Autogenous anticoagulated blood (50 cc) was extracted from each patient and centrifuged for 15 min (3000 round/minute) to separate into PRP and platelet poor plasma. The platelet poor plasma was disposed of, while the PRP was recentrifuged. The result was a noncellular concentrate of plasma, which has a platelet concentrate reaching 8 to 10 times that of blood baseline.
Under complete aseptic conditions, 5 cc of the previously prepared PRP were injected into the most tender part of the heel (medial side of the heel in relation to the medial tubercle of calcaneus). Injection was done using a peppering technique (single skin puncture and multiple injection in the plantar fascia). The patient was observed for 15–20 min after injection then discharged.
Patients were instructed to limit their activities and keep the injected limb elevated for 48 hr after injection. On the third day, a rehabilitation program was commenced, including 2 wk of plantar fascia and Achilles tendon stretching exercises followed by 4 wk of strengthening exercises. Patients were allowed to return to their normal activities including practicing sports. Three months after injection patients were reevaluated using the PFPS and FFI. The patients who had not improved proceeded to surgery (group B).
All surgeries were performed with the patient under spinal anesthesia with a thigh tourniquet inflated 100 mm Hg above the systolic pressure. Patients were positioned supine with the ipsilateral knee and hip semiflexed. A 5–6 cm medial incision was made, starting 1 cm distal and posterior to the tip of the medial malleolus and ending at the junction between the dorsal and plantar skin transition of the medial foot (Figure 1). Subcutaneous tissue was retracted, and the superficial fascia above the abductor hallucis muscle and the inferior part of the flexor retinaculum were incised, exposing the muscle and the neurovascular bundle (Figure 2). The muscle was retracted proximally and distally, and taut deep fascia between the inferior portion of the abductor hallucis and the medial margin of quadratus plantae was incised and excised, releasing Baxter's nerve, making sure it was released throughout its course (Figure 3). The superficial and deep surfaces of the medial plantar fascia were exposed and the medial portion of the plantar fascia incised towards the calcaneal tuberosity, sparing the lateral half of the plantar fascia; a 0.5-cm portion of the medial planter fascia was excised (Figure 4). The calcaneal spur is theoretically a cause of compression of the Baxter nerve, so it was removed with care not to injure the nerve. The medial calcaneal tubercle and surrounding bone were then drilled using a 2.7-mm drill bit (4 to 5 drills holes 1 cm deep and 3–5 mm apart). The tourniquet was then deflated and hemostasis ensured followed by closure in layers. A bulky dressing and below-knee back slab were applied.
Figure 2.
Incision of fascia over the abductor hallucis and inferior part of the flexor retinaculum, exposing the muscle and neurovascular bundle.
(A and B) Retracting the abductor hallucis muscle both proximally and distally, exposing and releasing the taut fascia beneath, thus releasing Baxter's nerve (C ).
Patients were discharged on the next postoperative day, stitches were removed the third week, and a below-knee cast was applied. Patients were encouraged to start partial weight bearing in the below-knee cast for 3 wk, proceeding gradually to full weight-bearing. Six weeks postoperatively the cast was removed and physical therapy begun, with stretching and strengthening rehabilitation program for 6 wk more. Six-months postoperatively patients were evaluated using PFPS and FFI.
Fourteen (58.3%) patients (seven men and seven women) with an average age 42.5 yr showed marked improvement 3 mo after injection, with improvement of their PFPS from 79.15 (range, 71.8 to 83.8) to 22.3 (range, 15.4 to 25.5) and improvement of the FFI from 160.42 (range, 155 to 166) to 30.4 points (range, 23 points to 38 points; Table 1).
Of the 14 patients, 11 (78.5%) had no functional limitations 3 mo after injection, while three (21.5%) had minimal activity limitations. Nevertheless, all patients were satisfied with the results.
Ten (41.7%) patients (seven men and three women) with an average age of 41.3 yr (34 to 53 yr) did not have marked improvement three months after injection and were still complaining of medial-side heel pain that was worse in the morning and restriction of their daily activities. Group B PFPS changed from 80.4 (range, 74.6 to 83.8) to 60.8 (range, 55.4 to 63.8), and the FFI changed from 168.6 (range, 161 to 179 ) to 143.4 (range, 122 to 155; Table 2)
Group B was further evaluated by MRI of the foot. In all 10 patients, MRI evidence of plantar fasciitis was present in the form of edematous changes in the proximal plantar aponeurosis with reactive edema in the adjacent calcaneus appearing on the sagittal STIR images. Nine patients had edema and volumeric atrophy in the abductor digiti minimi muscle belly, presenting as high-intensity signal on coronal and axial images, which corresponded to entrapment of the first branch of lateral planter nerve (Baxter's nerve).
Group B patients underwent surgical treatment in the form of decompression of the first branch of the lateral plantar nerve with partial medial plantar fasciotomy and drilling of the calcaneus. The postoperative PFPS improved from 60.8 (range, 55.4 to 63.8) to 21.8 (range, 16.4 to 25.6), and the postoperative FFI improved from 143.4 (range, 122 to 155) to 38 (range, 31 to 52) (Table 3). Eight patients (80%) had no functional limitations 6 mo after surgery. One patient reported only minimal functional limitations and one patient needed to use a silicone heel cup permanently.
One patient had wound dehiscence and was managed by repeated dressing, and secondary suturing was done under local anesthesia. Nine patients were satisfied with the results 6 mo postoperatively while one patient was fairly satisfied with the results.
The first line for treatment of heel pain should be nonsurgical including nonsteroidal anti-inflammatory medication, physical therapy, plantar fascia and Achilles tendon stretching exercises, shoes inserts, night splints, and even a period of immobilization. A bit more invasive nonsurgical procedures also can be used, such as local corticosteroid injection, which has been proven to have significant short-term pain relief at 4 wk after injection and insignificant pain relief at 3 mo after injection.[3,4] Moreover, a corticosteroid injection has reported complications, such as as fat pad atrophy and rupture of the plantar fascia.[2] Over the past few years Botulinum toxin A (BTX-A) has been used in treatment of chronic heel pain with recent clinical trials evaluating its efficacy.[5,6] Extracorporeal shock wave therapy also has been used for treatment of heel pain, with a success rate reaching 60% to 80%.[7]PRP injection has recently gained popularity in the management of muscle and tendon injuries and degeneration. PRP has six to eight times the normal level of growth factors,[8] which will result in fibrocyte migration, initiating a healing response necessary to reverse the degenerative process in the plantar fascia.[9] With no reported complications, such as with steroid injections, and the elimination of tissue rejection and blood disease transmission by use of autologous blood,[10] PRP injection provides significant improvement in pain and function, and this improvement is maintained over time.
In this study 14 patients of 24 (58.3%) patients had significant pain and functional improvement after PRP injection. Although three patients of the 14 (21.5%) had minimal activity limitations, all patients were satisfied with the results. Although other PRP injection studies showed a higher success rate reaching 88% in some studies,[10] our low success rate of injection may be related to the presence of other causes of heel pain than plantar fasciitis such as nerve entrapment and chronicity of symptoms.
Entrapment of the first branch of the lateral plantar nerve (Baxter's nerve) is an elusive cause of chronic heel pain that accounts for about 20% to 30% of the cases of heel pain.[11] Baxter's nerve is a mixed nerve that originates from lateral plantar nerve beneath the deep fascia of abductor hallucis muscle, carrying sensation from the calcaneal periosteum and supplying the abductor digiti mini muscle.[12,13] Baxter's nerve has two sites where it can become entrapped; the first is between the deep fascia beneath abductor hallucis muscle and the medial border of quadratus plantae; the second is anterior to the medial calcaneal tuberosity where it can be compressed by a calcaneal spur or thickened plantar fascia.[13] Nerve entrapment produces symptoms that are indistinguishable from the symptoms of plantar fascitis and often is overlooked from other causes of heel pain, and weakness of abductor digiti minimi is difficult to detect clinically and electrodiagnostic studies are inconclusive in heel pain. MRI is used to detect abnormalities of abductor digiti mini, which correspond to Baxter's nerve entrapment.[14,15]Nerve entrapment should be considered if chronic heel pain persists for more than 6 mo with no significant improvement after conservative treatment. In these cases freeing the nerve improves the patient symptoms.[16] The release should include all possible sites of entrapment: the deep fascia of the abductor hallucis, thickened medial plantar fascia, and calcaneal spur. Adding calcaneal drilling to the release decreases the calcaneal intraosseous pressure, which also may be cause of heel pain.
The surgical technique used in this study included release of the two entrapment sites of Baxter's nerve, excision of the calcaneal spur, and calcaneal drilling. This procedure treats most etiologies of heel pain, thus improving the patient postoperative satisfaction.[17] Baxter and Pfeffer[18]reported an 89% improvement of heel symptoms in patients treated with surgical decompression of the lateral planter nerve. Sadek et al.[19]performed release of the lateral plantar nerve associated with calcaneal drilling for treatment of chronic heel pain and reported a 93% improvement. Their results are comparable to our study.
In conclusion, conservative methods are the first-line treatment of heel pain, providing an 80% to 90% improvement rate.[1] Figure 5 shows the treatment algorithm. Persistence of symptoms for more than 6 mo may require PRP injection. In our study, PRP injection provided a safe, reliable method with 50% to 60% of patients showing improvement. Failure to obtain significant improvement is an indication for surgical intervention, with release of Baxter's nerve, medial plantar fasciectomy, and calcaneal drilling providing a satisfactory outcome.
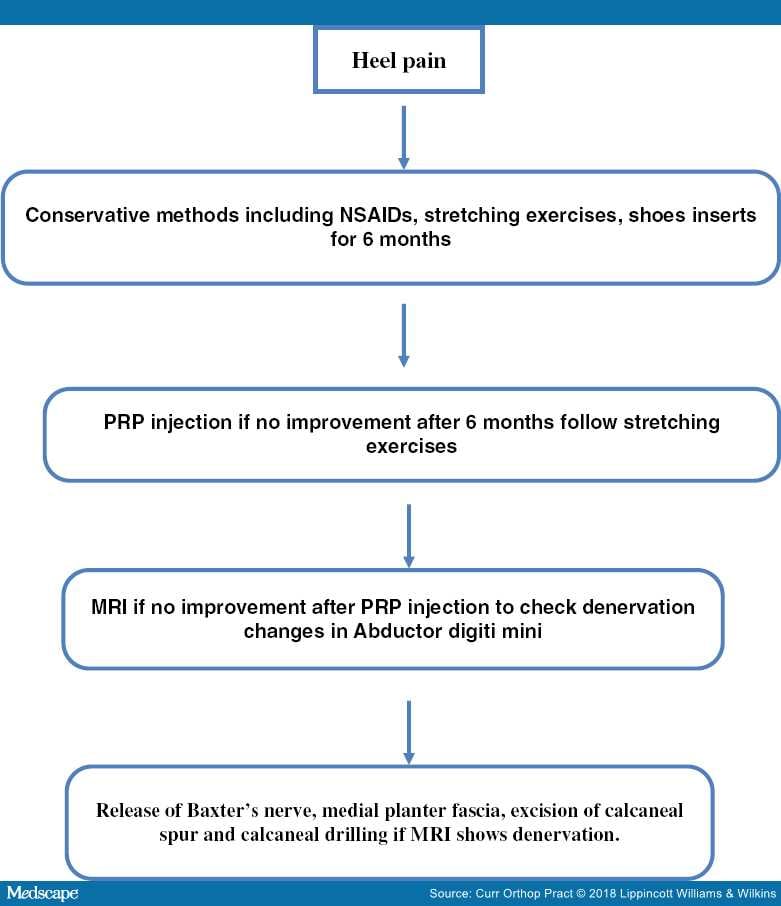
Figure 5.Treatment algorithm.