- 1.
Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, Dragomir A, Kalsbeek WD, Luta G, Jordan JM (2008) Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 59(9):1207–1213. https://doi.org/10.1002/art.24021
Article PubMed PubMed Central Google Scholar
- 2.
Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, Carr A, Beard D (2018) Knee replacement. Lancet (London, England) 392(10158):1672–1682. https://doi.org/10.1016/s0140-6736(18)32344-4
Article Google Scholar
- 3.
Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A, Kent S, TOPKAT Study Group (2019) The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet 394(10200):746–756. https://doi.org/10.1016/S0140-6736(19)31281-4
Article PubMed PubMed Central Google Scholar
- 4.
Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP (2009) Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 16(6):473–478. https://doi.org/10.1016/j.knee.2009.04.006
Article PubMed Google Scholar
- 5.
Peersman G, Verhaegen J, Favier B (2019) The forgotten joint score in total and unicompartmental knee arthroplasty: a prospective cohort study. Int Orthop 43(12):2739–2745. https://doi.org/10.1007/s00264-019-04342-w
Article PubMed Google Scholar
- 6.
Johal S, Nakano N, Baxter M, Hujazi I, Pandit H, Khanduja V (2018) Unicompartmental knee arthroplasty: the past, current controversies, and future perspectives. J Knee Surg 31(10):992–998. https://doi.org/10.1055/s-0038-1625961
Article PubMed Google Scholar
- 7.
Kleeblad LJ, Borus TA, Coon TM, Dounchis J, Nguyen JT, Pearle AD (2018) Midterm survivorship and patient satisfaction of robotic-arm-assisted medial unicompartmental knee arthroplasty: a multicenter study. J Arthroplasty 33(6):1719–1726. https://doi.org/10.1016/j.arth.2018.01.036
Article PubMed Google Scholar
- 8.
Baker P, Jameson S, Critchley R, Reed M, Gregg P, Deehan D (2013) Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am 95(8):702–709. https://doi.org/10.2106/jbjs.l.00520
Article PubMed Google Scholar
- 9.
Witjes S, Hoorntje A, Koenraadt KLM, Kerkhoffs GMMJ, van Geenen RCI (2019) Higher function scores and satisfaction in patients with anteromedial osteoarthritis compared with other wear patterns of the knee: 2 years after both total and unicondylar knee arthroplasties. J Knee Surg. https://doi.org/10.1055/s-0039-1683925
Article PubMed Google Scholar
- 10.
Canovas F, Dagneaux L (2018) Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res 104(1s):S41-s46. https://doi.org/10.1016/j.otsr.2017.04.017
CAS Article PubMed Google Scholar
- 11.
Barlow T, Griffin D, Barlow D, Realpe A (2015) Patients’ decision making in total knee arthroplasty: a systematic review of qualitative research. Bone Joint Res 4(10):163–169. https://doi.org/10.1302/2046-3758.410.2000420
CAS Article PubMed PubMed Central Google Scholar
- 12.
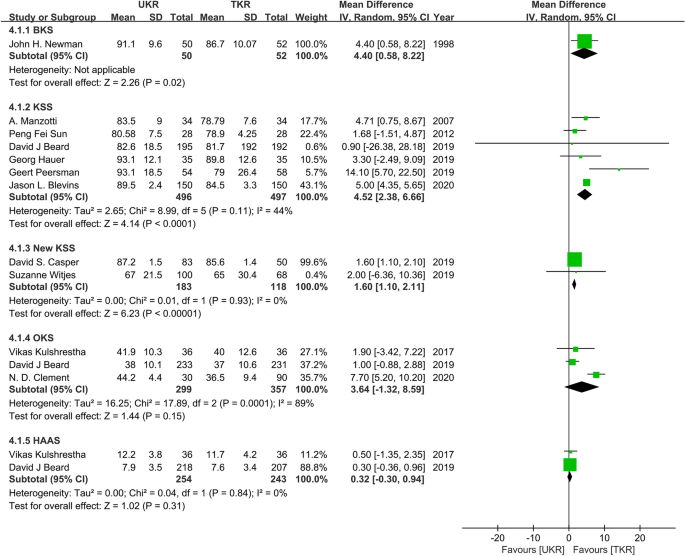
Blevins JL, Carroll KM, Burger JA, Pearle AD, Bostrom MP, Haas SB, Sculco TP, Jerabek SA, Mayman DJ (2020) Postoperative outcomes of total knee arthroplasty compared to unicompartmental knee arthroplasty: a matched comparison. Knee. https://doi.org/10.1016/j.knee.2019.12.005
Article PubMed Google Scholar
- 13.
Kulshrestha V, Datta B, Kumar S, Mittal G (2017) Outcome of unicondylar knee arthroplasty vs total knee arthroplasty for early medial compartment arthritis: a randomized study. J Arthroplasty 32(5):1460–1469. https://doi.org/10.1016/j.arth.2016.12.014
Article PubMed Google Scholar
- 14.
Price AJ, Svard U (2011) A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469(1):174–179. https://doi.org/10.1007/s11999-010-1506-2
Article PubMed Google Scholar
- 15.
Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J (2015) Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25(5):799–806. https://doi.org/10.1007/s00590-015-1610-9
Article PubMed Google Scholar
- 16.
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1811–1822. https://doi.org/10.1007/s00167-017-4817-y
Article PubMed Google Scholar
- 17.
Wilson HA, Middleton R, Abram SGF, Smith S, Alvand A, Jackson WF, Bottomley N, Hopewell S, Price AJ (2019) Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ 364:l352. https://doi.org/10.1136/bmj.l352
Article PubMed PubMed Central Google Scholar
- 18.
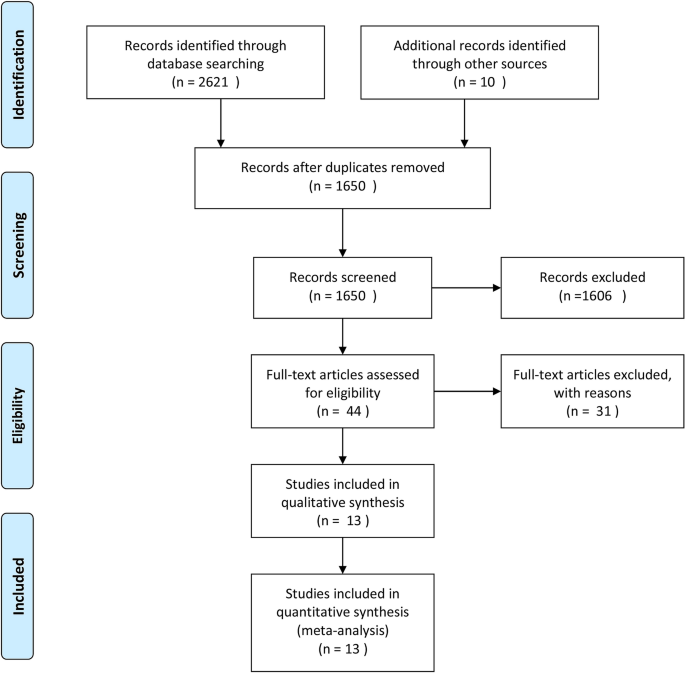
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Article PubMed PubMed Central Google Scholar
- 19.
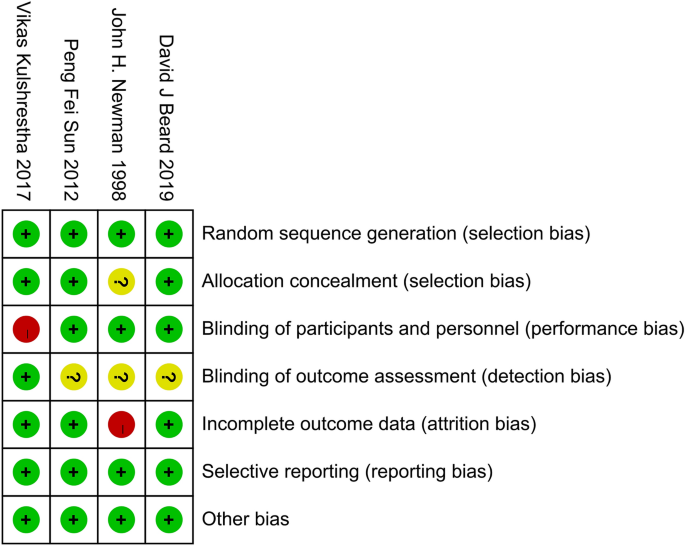
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928–d5928. https://doi.org/10.1136/bmj.d5928
Article PubMed PubMed Central Google Scholar
- 20.
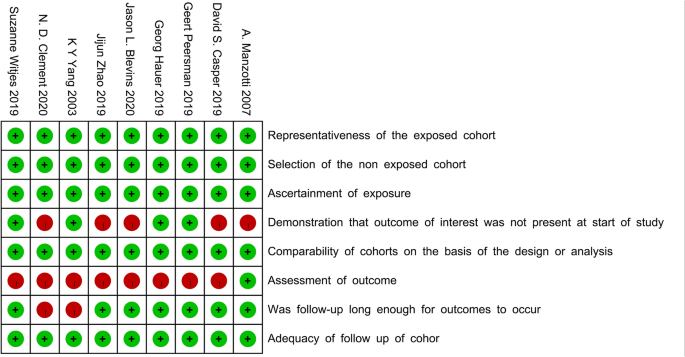
Margulis AV, Pladevall M, Riera-Guardia N, Varas-Lorenzo C, Hazell L, Berkman ND, Viswanathan M, Perez-Gutthann S (2014) Quality assessment of observational studies in a drug-safety systematic review, comparison of two tools: the Newcastle-Ottawa Scale and the RTI item bank. Clin Epidemiol 6:359–368. https://doi.org/10.2147/CLEP.S66677
Article PubMed PubMed Central Google Scholar
- 21.
Michailidou K (2018) Meta-analysis of common and rare variants. Methods Mol Biol 1793:73–88. https://doi.org/10.1007/978-1-4939-7868-7_6
CAS Article PubMed Google Scholar
- 22.
Lin L, Chu H (2018) Quantifying publication bias in meta-analysis. Biometrics 74(3):785–794. https://doi.org/10.1111/biom.12817
Article PubMed Google Scholar
- 23.
Clement ND, Bell A, Simpson P, Macpherson G, Patton JT, Hamilton DF (2020) Robotic-assisted unicompartmental knee arthroplasty has a greater early functional outcome when compared to manual total knee arthroplasty for isolated medial compartment arthritis. Bone Joint Res 9(1):15–22. https://doi.org/10.1302/2046-3758.91.bjr-2019-0147.r1
CAS Article PubMed PubMed Central Google Scholar
- 24.
Zhao J, Wu Z, Yu Y, Zhou Z, Feng D (2019) Comparison of unicompartmental knee arthroplasty and total knee arthroplasty on joint function in elderly patients with knee osteoarthritis. Int J Clin Exp Med 12(2):2072–2078
Google Scholar
- 25.
Hauer G, Sadoghi P, Bernhardt GA, Wolf M, Ruckenstuhl P, Fink A, Leithner A, Gruber G (2019) Greater activity, better range of motion and higher quality of life following unicompartmental knee arthroplasty: a comparative case–control study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-019-03296-3
Article PubMed PubMed Central Google Scholar
- 26.
Casper DS, Fleischman AN, Papas PV, Grossman J, Scuderi GR, Lonner JH (2019) Unicompartmental knee arthroplasty provides significantly greater improvement in function than total knee arthroplasty despite equivalent satisfaction for isolated medial compartment osteoarthritis. J Arthroplasty 34(8):1611–1616. https://doi.org/10.1016/j.arth.2019.04.005
Article PubMed Google Scholar
- 27.
Newman JH, Ackroyd CE, Shah NA (1998) Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br 80(5):862–865. https://doi.org/10.1302/0301-620x.80b5.8835
CAS Article PubMed Google Scholar
- 28.
Sun PF, Jia YH (2012) Mobile bearing UKA compared to fixed bearing TKA: a randomized prospective study. Knee 19(2):103–106. https://doi.org/10.1016/j.knee.2011.01.006
Article PubMed Google Scholar
- 29.
Manzotti A, Confalonieri N, Pullen C (2007) Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop 31(3):315–319. https://doi.org/10.1007/s00264-006-0184-x
CAS Article PubMed Google Scholar
- 30.
Yang KY, Wang MC, Yeo SJ, Lo NN (2003) Minimally invasive unicondylar versus total condylar knee arthroplasty—early results of a matched-pair comparison. Singapore Med J 44(11):559–562
CAS PubMed Google Scholar
- 31.
Weale AE, Murray DW, Newman JH, Ackroyd CE (1999) The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br 81(5):790–795. https://doi.org/10.1302/0301-620x.81b5.9590
CAS Article PubMed Google Scholar
- 32.
Newman J, Pydisetty RV, Ackroyd C (2009) Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br 91(1):52–57. https://doi.org/10.1302/0301-620x.91b1.20899
CAS Article PubMed Google Scholar
- 33.
Kim KT, Lee S, Lee JS, Kang MS, Koo KH (2018) Long-term clinical results of unicompartmental knee arthroplasty in patients younger than 60 years of age: minimum 10-year follow-up. Knee Surg Relat Res 30(1):28–33. https://doi.org/10.5792/ksrr.17.025
Article PubMed PubMed Central Google Scholar
- 34.
van der List JP, Chawla H, Villa JC, Pearle AD (2017) The Role of patient characteristics on the choice of unicompartmental versus total knee arthroplasty in patients with medial osteoarthritis. J Arthroplasty 32(3):761–766. https://doi.org/10.1016/j.arth.2016.08.015
Article PubMed Google Scholar
- 35.
Siman H, Kamath AF, Carrillo N, Harmsen WS, Pagnano MW, Sierra RJ (2017) Unicompartmental knee arthroplasty vs total knee arthroplasty for medial compartment arthritis in patients older than 75 years: comparable reoperation, revision, and complication rates. J Arthroplasty 32(6):1792–1797. https://doi.org/10.1016/j.arth.2017.01.020
Article PubMed Google Scholar
- 36.
Na SE, Ha CW, Lee CH (2012) A new high-flexion knee scoring system to eliminate the ceiling effect. Clin Orthop Relat Res 470(2):584–593. https://doi.org/10.1007/s11999-011-2203-5
Article PubMed Google Scholar
- 37.
Hansen EN, Ong KL, Lau E, Kurtz SM, Lonner JH (2019) Unicondylar knee arthroplasty has fewer complications but higher revision rates than total knee arthroplasty in a study of large united states databases. J Arthroplasty 34(8):1617–1625. https://doi.org/10.1016/j.arth.2019.04.004
Article PubMed Google Scholar
- 38.
Dyrhovden GS, Lygre SHL, Badawy M, Gothesen O, Furnes O (2017) Have the causes of revision for total and unicompartmental knee arthroplasties changed during the past two decades? Clin Orthop Relat Res 475(7):1874–1886. https://doi.org/10.1007/s11999-017-5316-7
Article PubMed PubMed Central Google Scholar
- 39.
Liddle AD, Pandit H, Judge A, Murray DW (2016) Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Joint Surg Am 98(1):1–8. https://doi.org/10.2106/jbjs.n.00487
Article PubMed Google Scholar
- 40.
Hamilton TW, Rizkalla JM, Kontochristos L, Marks BE, Mellon SJ, Dodd CAF, Pandit HG, Murray DW (2017) The interaction of caseload and usage in determining outcomes of unicompartmental knee arthroplasty: a meta-analysis. J Arthroplasty 32(10):3228-3237.e3222. https://doi.org/10.1016/j.arth.2017.04.063
Article PubMed Google Scholar
- 41.
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S, Munzinger U, Drobny T (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35(10):1688–1695. https://doi.org/10.1177/0363546507303562
Article PubMed Google Scholar
- 42.
Scott CEH, Wade FA, MacDonald D, Nutton RW (2018) Ten-year survival and patient-reported outcomes of a medial unicompartmental knee arthroplasty incorporating an all-polyethylene tibial component. Arch Orthop Trauma Surg 138(5):719–729. https://doi.org/10.1007/s00402-018-2908-y
Article PubMed PubMed Central Google Scholar