Abstract
Purpose
The optimal surgical timeframe for neurological recovery in traumatic spinal cord injury (tSCI) still remains unknown. Recent guidelines have recommended performing surgery within 24 h for all patients with tSCI regardless of initial neurological deficit. It remains unclear whether patients with complete, incomplete tSCI, or traumatic central cord injury (TCCI) will experience the same degree of improvement after urgent surgical intervention. We investigated if the severity of initial neurological injury influenced surgeons on their decision-making of surgical timing in tSCI.
Methods
With a web-based survey, we investigated the current opinion in The Netherlands on timing of surgical decompression and stabilization, depending on the initial degree of neurological injury.
Results
Surgeons prefer to perform more urgent surgery for incomplete tSCI compared to complete tSCI. In addition, 43% of patients with complete tSCI are not preferably operated within the recommended 24 h. Even though TCCI is the most common form of incomplete tSCI, these patients are preferably managed less urgently than patients with other types of incomplete tSCI.
Conclusion
The severity of initial neurological injury seems to play an important role in the urgency of surgical timing for tSCI. A substantial number of patients with complete tSCI are not preferably treated within the recommended surgical timeframe, while patients with incomplete tSCI are preferably operated far more urgent than recommended in the current guidelines.
Keywords
Spinal cord injuries Timing Decompression Stabilization Survey Spine trauma
Introduction
Traumatic spinal cord injury (tSCI) is a devastating event, affecting a patient’s life in innumerable ways [1]. Surgical decompression seems to have a beneficial effect on the neurological outcome in the acutely injured spinal cord [2, 3]. However, the optimal surgical timeframe for maximizing neurological recovery remains unclear, as well as the impact of urgent surgery in complete compared to incomplete tSCI [4, 5, 6].
The Surgical Timing in Acute Spinal Cord Injury Study study (STASCIS) was the first large, international, prospective cohort study in cervical tSCI patients to investigate the effect of surgical timing on neurological outcome [3]. This study showed a beneficial effect on neurological outcome when surgical decompression and stabilization was performed within 24 h after injury compared to surgery performed after 24 h, in both patients with complete and incomplete tSCI.
Recently, some smaller studies have also confirmed that neurological recovery is not only limited to patients with incomplete tSCI [7, 8]. This effect was also seen in complete tSCI when surgery was performed urgently [4]. In addition, recent international guidelines recommend performing surgery within 24 h for tSCI regardless of initial neurological status [9, 10].
While the optimal surgical timeframe is still unclear, current studies are investigating even earlier surgical timeframes [5, 6, 8].
We investigated to what extent recent international guidelines are implemented in daily practice and whether the initial neurological exam has an impact on the current decision-making in surgical management of tSCI patients [9].
Methods
Since the surgical treatment of patients with tSCI in The Netherlands is primarily performed in multidisciplinary teams, a multidisciplinary group from three university medical centers (VU University Medical Center and Academic Medical Center both in Amsterdam, and University Medical Center Utrecht), consisting of two neurosurgeons, a trauma surgeon and two orthopedic surgeons, developed a short, web-based, survey on the timing of surgery in tSCI patients (see supplementary appendix). We conducted the survey between November 2016 and January 2017. The survey was sent to all 138 Dutch neurosurgeons, member of the Dutch Society of Neurological Surgeons of which 59 were also member of the Dutch Spine Society (DSS). In addition, the survey was sent to all 88 orthopedic surgeons who are members of the DSS and 13 trauma surgeons at the VU University Medical Center and University Medical Center in Groningen, where trauma surgeons participate in acute surgical management of patients with tSCI.
The survey comprised of 15 questions, divided into three parts, and focused on the influence of the level and severity of neurological injury on surgical timing. The first part consisted of seven general questions on case volume and role of the surgeon in the management of tSCI patients. The second part contained five questions regarding one hypothetical case with traumatic spinal cord injury with traumatic instability of the spine and four different degrees of neurological injury [ASIA A, B, C/D, and traumatic central cord injury (TCCI)], and a second hypothetical case with traumatic central cord injury without spinal instability. Surgeons were asked to choose a specific timeframe to perform surgical decompression and stabilization in these hypothetical patients, who were hemodynamically stable and did not have any contra-indications for urgent surgery. The surgical timing was categorized as ultra-early (directly from the ER or within 8–12 h after trauma), early (within 24 h, not specifically < 12 h), late (within 72 h), or other (e.g., timing depending on logistics or deterioration).
The third part consisted of three questions of surgical timing and the level of injury, since most of the evidence for urgent surgical decompression comes from studies in cervical tSCI patients only. Respondents were asked to comment on their preferred surgical timing for each case.
ASIA classification
|
ASIA classification |
|
|---|---|
|
ASIA A |
Complete spinal cord motor injury, including complete sensory injury |
|
ASIA B |
Complete spinal cord motor injury with preservation of sacral sensation (S4, 5) |
|
ASIA C |
Incomplete spinal cord motor injury, with < MRC3 (motion against gravity is not possible) in > 50% of all key muscles |
|
ASIA D |
Incomplete spinal cord motor injury, with ≥ MRC3 (motion against gravity is possible) in > 50% of all key muscles |
|
ASIA E |
No motor or sensory spinal cord injury |
|
TCCI |
Motor impairment is worse in upper extremities than in lower extremities (10 MRC points less in arms than in legs) |
Traumatic central cord injury (TCCI), the most common form of an incomplete (ASIA C or D) spinal cord injury, is characterized by motor impairment in upper extremities worse than in lower extremities. Since a clear distinction is made in daily practice between ASIA C/D and TCCI, we asked respondents to comment separately on their surgical timing for this specific subtype of incomplete tSCI. We made a distinction between TCCI with and without spinal instability, as TCCI more often presents in patients with preexisting spinal canal stenosis and a mild trauma. This last entity is usually thought to harbor an equal, or better, prognosis with non-operative management than surgery.
We analyzed all responses on surgical timing for all grades of tSCI and stratified responders by specialty and whether they had a spinal subspecialization.
Results
With 88 participants [59/88 (67%) neurosurgeons, 23/88 (26%) orthopedic surgeons, and 6/88 (7%) trauma surgeons], there was an overall response rate of 37% of which 67% were spinal subspecialized. Spinal surgery was the subspecialty of 31/59 (53%) neurosurgeons, 23/23 (100%) orthopedic surgeons, and 5/6 (83%) trauma surgeons. Thirty-eight (43%) respondents reported an estimated annual incidence of 10–20 patients with tSCI at their center and 21 (24%) an estimated annual incidence of > 20 tSCI patients (Suppl. 1).
Timing of surgery in tSCI and relation to the severity of neurological injury
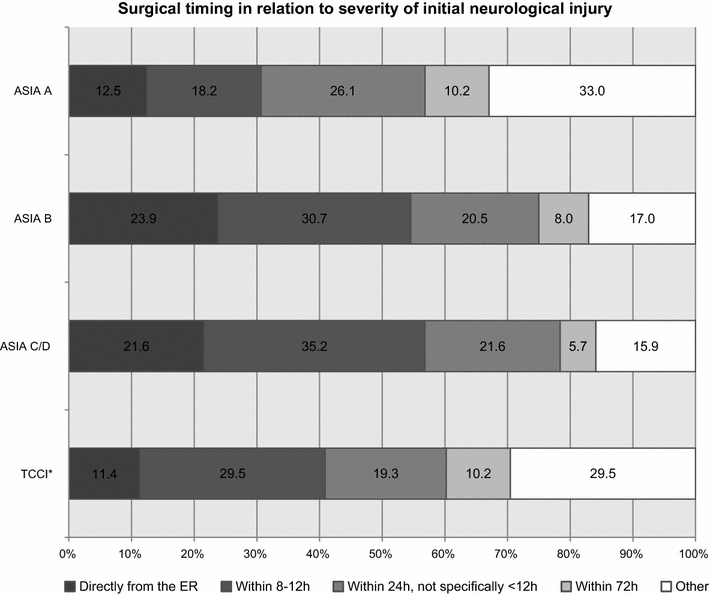
Surgical timing in relation with severity of initial neurological injury. Other includes respondents who did not choose a specific timeframe, found logistics or deterioration important or were not involved in the decision-making on surgical timing. TCCI*: TCCI with spinal column/discoligamentous injury
For incomplete tSCI, a substantial number of surgeons (56%) prefer to perform ultra-early (< 12 h) surgery, in contrast to 31% for complete ASIA A tSCI.
Timing of surgery in traumatic central cord injury (TCCI)
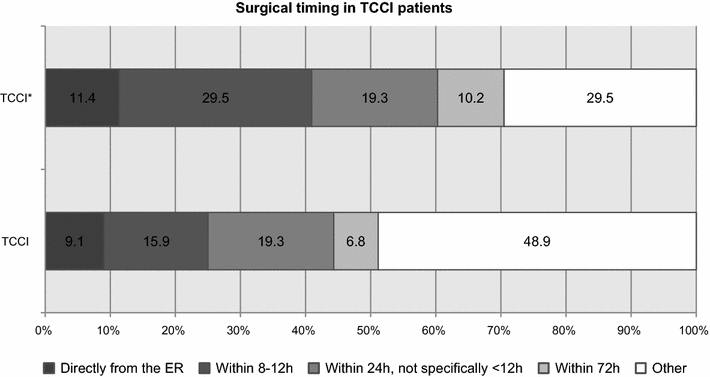
Surgical timing in TCCI. TCCI*: TCCI with spinal column/discoligamentous injury. Other includes respondents who did not choose a specific timeframe, found logistics or deterioration important or were not involved in the decision-making on surgical timing
Timing in relationship to spinal subspecialization and surgical specialty
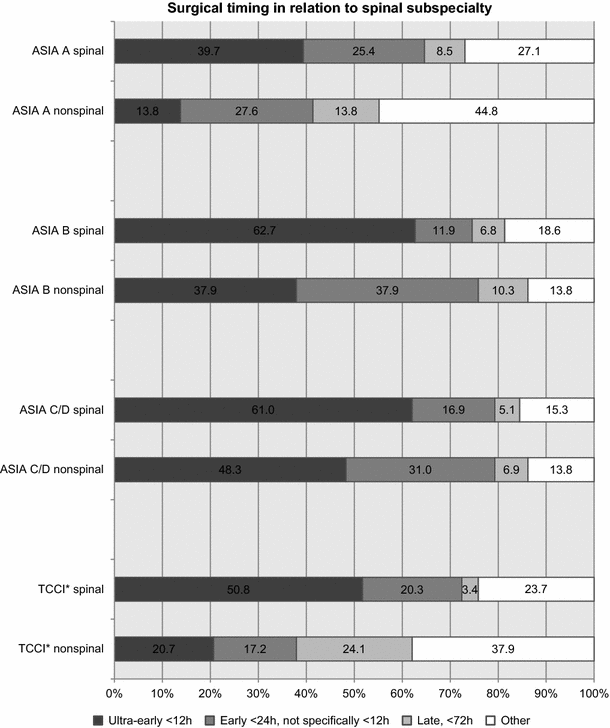
Surgical timing in relation with spinal subspecialization. TCCI*: TCCI with spinal column/discoligamentous injury
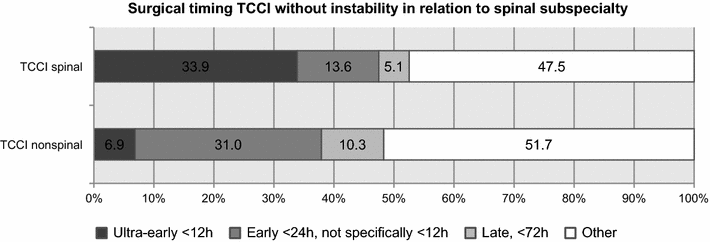
Preferred surgical timing in TCCI without spinal instability. Other includes surgeons who were not involved in the treatment of these patients or found logistics or deterioration important for surgical timing
Preferred surgical timing in patients with ASIA A, B, C/D, central-cord-type injury dependent on specialty and spinal subspecialization, TCCI*
|
Surgical timing of spinal surgeons in relation with specialty |
||||
|---|---|---|---|---|
|
Directly from the ER (%) |
Ultra-early (< 12 h) (%) |
Early (< 24 h) (%) |
Total |
|
|
ASIA A |
||||
|
Neurosurgeon |
5 (16) |
5 (16) |
8 (26) |
18/31 |
|
Orthopedic surgeon |
6 (26) |
6 (26) |
5 (22) |
17/23 |
|
Trauma surgeon |
0 |
1 (20) |
2 (40) |
3/5 |
|
ASIA B |
||||
|
Neurosurgeon |
11 (35) |
8 (26) |
3 (10) |
22/31 |
|
Orthopedic surgeon |
8 (35) |
9 (39) |
1 (4) |
18/23 |
|
Trauma surgeon |
0 |
1 (20) |
3 (60) |
4/5 |
|
ASIA C/D |
||||
|
Neurosurgeon |
12 (39) |
8 (26) |
6 (19) |
26/31 |
|
Orthopedic surgeon |
4 (17) |
11 (48) |
1 (4) |
16/23 |
|
Trauma surgeon |
0 |
1 (20) |
3 (60) |
4/5 |
|
TCCI* |
||||
|
Neurosurgeon |
5 (16) |
10 (32) |
9 (29) |
24/31 |
|
Orthopedic surgeon |
4 (17) |
10 (43) |
1 (4) |
15/23 |
|
Trauma surgeon |
0 |
1 (20) |
2 (40) |
4/5 |
Timing of surgery in relation with the level of injury and ideal surgical timing
The majority of the respondents applied the same surgical timing, as for cervical injuries, in patients with thoracic and conus/cauda injury (83 and 74%, respectively). Two-third (55/88) of the respondents would not ideally perform surgery for any form of tSCI in a more urgent matter. Most of the respondents who commented on their choice (13/55) found the evidence too scant to change their current time management for tSCI.
Discussion
Our survey showed that the severity of initial neurological injury seems to play an important role in the decision-making for timing of surgical decompression, since patients with incomplete tSCI are preferably operated in a more urgent fashion than patients with complete tSCI. While patients with incomplete tSCI are preferably treated more urgent than the recommended international guideline, only 57% of patients with complete tSCI are preferably surgically treated within 24 h. In contrast to patients with incomplete tSCI, patients with traumatic central cord injury (TCCI) are preferably treated less urgently. In particular, TCCI patients without spinal instability are generally treated far more conservatively.
An international survey administered before the STASCIS study showed a more urgent approach compared to our findings [12]. They found that surgeons preferred to perform surgery within 24 h in 85.3–96.3% of all tSCI patients and 65–87.5% within 12 h. This is in contrast to 57–78% of Dutch surgeons who prefer to operate within 24 h and 30.7–56.8% within 12 h. Other surveys that were carried out after the STASCIS study also show a less aggressive approach compared to the prior international survey [13, 14]. One of which was administered in 2013 in Canada, 50–93.3% of all surgeons preferred to perform surgery within 24 h and 16.6–55% within 12 h [13]. Another survey performed in 2012 in the UK showed that 30–61% of all surgeons also preferred to perform surgery within 12 h in tSCI [14].
We observed that the initial neurological status plays an important role in the timing of surgical intervention for tSCI. In The Netherlands, 57% of the surgeons prefer to perform surgery within 24 h for ASIA A, 75% for ASIA B, and 78% for ASIA C/D. A less urgent approach for complete spinal cord injury was also present in the UK survey from 2012 [14]. In contrary, the Canadian survey from 2013 showed that 93.3% of the surgeons preferred to perform surgery within 24 h for ASIA A/B, 70% for ASIA C, and 50% for ASIA D [13]. This suggests that patients with complete tSCI are treated different from patients with incomplete tSCI internationally [12, 13, 14, 15]. However, although TCCI is the most common form of incomplete tSCI, these patients are treated differently in The Netherlands than patients with other forms of incomplete tSCI. Moreover, TCCI patients without spinal instability were preferably treated far less urgently (44% < 24 h vs. 60.2%). This implies that surgical treatment for patients with TCCI is heterogeneous and mostly depends on the presence of spinal instability. Surgeons have been skeptical about the role of urgent surgery for TCCI, since a substantial amount of patients with TCCI will improve spontaneously, independent of surgery [9, 16]. However, full recovery is not always present and about a fourth of all patients will experience neurological deterioration and still requires surgery. Since the distinction between TCCI and incomplete tSCI is not always clear, and discoligamentous injury is not always ruled out in the early stages by MRI, it is difficult to draw conclusions that patients with TCCI will not benefit from urgent surgery in comparison to patients with other forms of incomplete tSCI [17, 18].
Surveys are inevitably accompanied by limitations. As participants of the survey were anonymous, homogeneity of the data could not be checked, nor were analyses between centers possible. Our survey showed that non-spinal subspecialized surgeons are less inclined to perform urgent surgery than their spinal subspecialized colleagues. A possible explanation for this less urgent approach could be a different interpretation of the current literature regarding timing of surgery for tSCI. On the other hand, spinal surgeons are independent of other colleagues and, therefore, may feel more comfortable in performing this type of surgery in an urgent fashion. In this survey, the preferred timing to perform a surgical decompression might not always correspond with the actual timing in day-to-day practice [13]. Nevertheless, the results from our survey still reflect the current opinion on surgical timing among all Dutch surgeons involved in the care of tSCI patients.
One might question whether the evidence for the current recommended timeframe (< 24 h) in the guidelines is robust enough, given the lack of hard evidence of superiority of this timeframe [9]. Although the STASCIS study showed a trend towards superiority of urgent (< 24 h) surgery for neurological recovery in tSCI, its statistical power has been seriously challenged [3, 19, 20]. Nor is there clear evidence supporting our current approach, where patients with complete tSCI are managed within different timeframes than patients with incomplete tSCI. Nevertheless, a substantial amount of surgeons seems to prefer to perform surgery in an even more urgent (< 12 h) fashion. Unfortunately, the evidence supporting urgent surgery has not become much clearer since the STASCIS study. Meanwhile, SCI patients are undergoing more operations at low-volume and non-trauma hospitals without a concomitant increase in survival, suggesting that the trend for urgent surgery might preclude immediate transfer to high-volume centers [21]. Currently, there is no robust evidence supporting the value of ultra-early surgery for incomplete tSCI, nor is there any hard evidence contradicting the benefit of urgent surgery for patients with complete tSCI.
In addition, the validity of using the ASIA scheme at the initial admission has been questioned, since a proper assessment of ASIA level is only possible after three different evaluations within 72 h. Possibly, the increase of spinal cord edema in the first 48 h after trauma, as demonstrated by temporal changes of MRI characteristics, plays an important role [22, 23, 24].
To improve the neurological outcome of tSCI patients, we, therefore, think that it is of utmost importance to set up one prospective international registry on surgical timing and outcome, given the rarity of these lesions. With such a registry, we could investigate our true current surgical timing and its impact on neurological outcome to treat patients on the best individual basis.
Conclusion
The severity of initial neurological injury seems to play an important role in the decision-making of surgical timing in tSCI. Current guidelines do not discriminate on timing of operation depending on the degree of tSCI. However, in current practice, a clear distinction is made, since patients with complete tSCI and TCCI are preferably managed less urgent than patients with incomplete tSCI.
Notes
Funding
No funds were received in support of this work. No relevant financial activities outside the submitted work.
Compliance with ethical standards
Conflict of interest
All authors report no conflict of interest and have no financial disclosures.
References
-
1.Post MWM, van Leeuwen CMC (2012) Psychosocial issues in spinal cord injury: a review. Spinal Cord 50(5):382–389CrossRefPubMedGoogle Scholar
-
2.Ropper AE, Ropper AH (2017) Acute spinal cord compression. N Engl J Med 376(14):1358–1369CrossRefPubMedGoogle Scholar
-
3.Fehlings MG et al (2012) Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS). PLoS One 7(2):e32037CrossRefPubMedPubMedCentralGoogle Scholar
-
4.Bourassa-Moreau E et al (2016) Do patients with complete spinal cord injury benefit from early surgical decompression? Analysis of neurological improvement in a prospective cohort study. J Neurotrauma 33(3):301–306CrossRefPubMedGoogle Scholar
-
5.Burke JF et al (2016) 182 ultra-early (< 12 hours) decompression improves recovery after spinal cord injury compared to early (12–24 hours) decompression. Neurosurgery 63(Suppl 1):172CrossRefGoogle Scholar
-
6.Biglari B et al (2016) Does surgical treatment within 4 hours after trauma have an influence on neurological remission in patients with acute spinal cord injury? Ther Clin Risk Manag 12:1339–1346CrossRefPubMedPubMedCentralGoogle Scholar
-
7.Jug M et al (2015) Neurological recovery after traumatic cervical spinal cord injury is superior if surgical decompression and instrumented fusion are performed within 8 hours versus 8 to 24 hours after injury: a single center experience. J Neurotrauma 32(18):1385–1392CrossRefPubMedGoogle Scholar
-
8.Grassner L et al (2016) Early decompression (< 8 h) after traumatic cervical spinal cord injury improves functional outcome as assessed by spinal cord independence measure after one year. J Neurotrauma 33(18):1658–1666CrossRefPubMedGoogle Scholar
-
9.Wilson JR et al (2016) 181 guidelines for the management of patients with spinal cord injury: the optimal timing of decompression. Neurosurgery 63(Suppl 1):172CrossRefGoogle Scholar
-
10.Fehlings MG et al (2017) A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: recommendations on the timing (≤ 24 hours versus > 24 hours) of decompressive surgery. Global Spine J 7(3 suppl):195S–202SCrossRefPubMedPubMedCentralGoogle Scholar
-
11.Maynard FMJ et al (1997) International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord 35(5):266–274CrossRefPubMedGoogle Scholar
-
12.Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B (2010) Current practice in the timing of surgical intervention in spinal cord injury. Spine 35(21 Suppl):S166–S173CrossRefPubMedGoogle Scholar
-
13.Glennie RA et al (2017) An analysis of ideal and actual time to surgery after traumatic spinal cord injury in Canada. Spinal Cord 55(6):618–623CrossRefPubMedGoogle Scholar
-
14.Werndle MC et al (2012) Variability in the treatment of acute spinal cord injury in the United Kingdom: results of a national survey. J Neurotrauma 29(5):880–888CrossRefPubMedGoogle Scholar
-
15.Samuel AM et al (2015) Analysis of delays to surgery for cervical spinal cord injuries. Spine (Phila Pa 1976) 40(13):992–1000CrossRefGoogle Scholar
-
16.Anderson KK et al (2015) Optimal timing of surgical decompression for acute traumatic central cord syndrome: a systematic review of the literature. Neurosurgery 77(Suppl 4):S15–S32CrossRefPubMedGoogle Scholar
-
17.Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF (2010) The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine (Phila Pa 1976) 35(21 Suppl):S180–S186CrossRefGoogle Scholar
-
18.van Middendorp JJ, Hosman AJF, Doi SAR (2013) The effects of the timing of spinal surgery after traumatic spinal cord injury: a systematic review and meta-analysis. J Neurotrauma 30(21):1781–1794CrossRefPubMedGoogle Scholar
-
19.van Middendorp JJ (2012) Letter to the editor regarding: ‘Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS)’. Spine J 12(6):540CrossRefPubMedGoogle Scholar
-
20.Toole JEO (2014) Timing of surgery after cervical spinal cord injury. World Neurosurg 82(7–8):1–2Google Scholar
-
21.Holland CM, Mazur MD, Bisson EF, Schmidt MH, Dailey AT (2017) Trends in patient care for traumatic spinal injuries in the United States: a national inpatient sample study of the correlations with patient outcomes from 2001 to 2012. Spine (Phila Pa 1976) 42(24):1923–1929CrossRefGoogle Scholar
-
22.Vaccaro AR et al (2013) AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 38(23):2028–2037CrossRefGoogle Scholar
-
23.Kalsi-Ryan S, Wilson J, Yang JM, Fehlings MG (2014) Neurological grading in traumatic spinal cord injury. World Neurosurg 82(3–4):509–518CrossRefPubMedGoogle Scholar
-
24.Rutges JPHJ, Kwon BK, Heran M, Ailon T, Street JT, Dvorak MF (2017) A prospective serial MRI study following acute traumatic cervical spinal cord injury. Eur Spine J 26(9):2324–2332CrossRefPubMedGoogle Scholar
Copyright information
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.