One of the major drawbacks of the lateral approaches to the hip introduced over the last decades [1, 2, 3] is that they affect the hip abductor muscles negatively. They come close to the branches of the superior gluteal nerve [4, 5, 6] where lesions can result in partial or total fatty degeneration of the gluteus medius, minimus and tensor fasciae latae.
Pfirrmann et al. reported a total fatty generation in result of a direct muscle damage or to failure to restore the gluteal insertion after a transgluteal approach [7]. Muscle atrophy is an important differential diagnosis relative to simple tendon tear in patients with limping, which may be caused also by damage to the superior gluteal nerve after lateral approach hip surgery [7]. In a prospective study of Ramesh et al. involving 81 consecutive patients who underwent lateral approach total hip arthroplasty, the abductor muscles of the hip were assessed electrophysiologically and clinically. Results showed that in nine patients, complete denervation occurred [4]. Barrack et al. states that sciatic nerve injury is the most common nerve injury following THA. Femoral nerve injury is mainly associated with an anterior approach, with a generally better prognosis than with sciatic nerve injury, while the superior gluteal nerve is at risk during the direct lateral approach [8].
Because the gluteus medius and minimus are the main abductors of the hip joint insufficiencies can lead to a decrease in pelvic stability. In severe cases, this can cause clinically relevant weakness and a positive Trendelenburg sign, the inability to stabilize the pelvis in the stance phase of the gait cycle. The resultant limping greatly reduces patient quality of life and is considered a major complication in total hip arthroplasty [9].
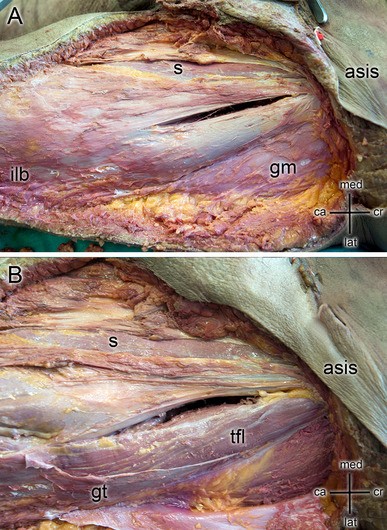
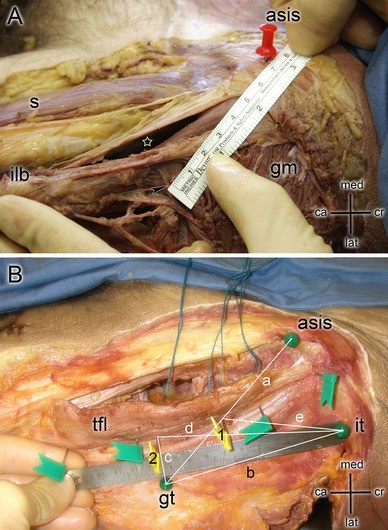
Therefore, attempts have been made to perform less-invasive total hip arthroplasty using muscle-preserving approaches such as the direct anterior approach [10, 11, 12]. In comparison to the Watson–Jones or anterolateral interval [13, 14, 15, 16, 17] the Smith–Peterson interval or direct anterior approach is an intramuscular and internerval approach [18, 19, 20, 21, 22, 23]. Although both intervals are muscle-preserving methods [9], only the direct anterior approach is truly internerval. The muscle medial, sartorius and rectus femoris, are innervated by branches of the femoral nerve, those lateral, tensor fasciae latae, gluteus medius and minimus are innervated by the superior gluteal nerve. In the anterior approach, access to the hip joint is obtained by passing between the sartorius (femoral nerve) and tensor fasciae latae (superior gluteal nerve) [24]. The gluteal nerve is the only motoric nerve that exits superior to piriformis muscle and then divides into a superior and an inferior branch [25]. It derives from the posterior braches of the ventral rami of the fourth and fifth lumbar and the first sacral spinal nerves. The gluteal nerve is supplying the gluteus medius, gluteus minimus, and tensor fasciae latae muscles. The gluteus medius and minimus muscle are both innervated by the superior and inferior braches. The terminal branches of the inferior branch are innervating tensor fasciae latea which runs anteriorly to it [26].
Retraction of soft tissue can exert considerable forces on the surrounding tissues especially in minimally invasive approaches, where only a small incision is given [27]. Retraction can cause significant damage to the tissue and result in postoperative acute or chronic pain—due to compression neuropraxia [28, 29, 30]. It is highly recommended to use special care with surgical instruments, especially retractors, to avoid excessive retraction. Excessive retraction can be exerted primarily during dislocation of the hip. Supporting the limb throughout the operation is highly recommended [31].
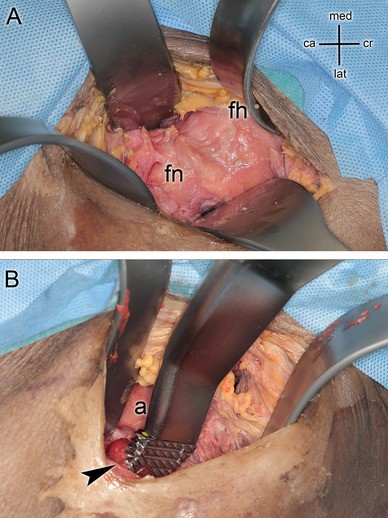
Our aim was to localize the superior gluteal nerve in relation to anatomical landmarks as the anterior superior iliac spine (ASIS), the greater trochanter (GT) and the iliac tubercle (IT). The gluteal nerve was exposed after instrumentation of hip arthroplasty via the direct anterior approach to visualize, if the nerve was injured by the direct anterior approach [20, 23, 32].