Cervical spine surgery may affect sagittal alignment parameters and induce accelerated degeneration of the cervical spine. Cervical sagittal alignment parameters of surgical patients will be correlated with radiological adjacent segment degeneration (ASD) and with clinical outcome parameters.
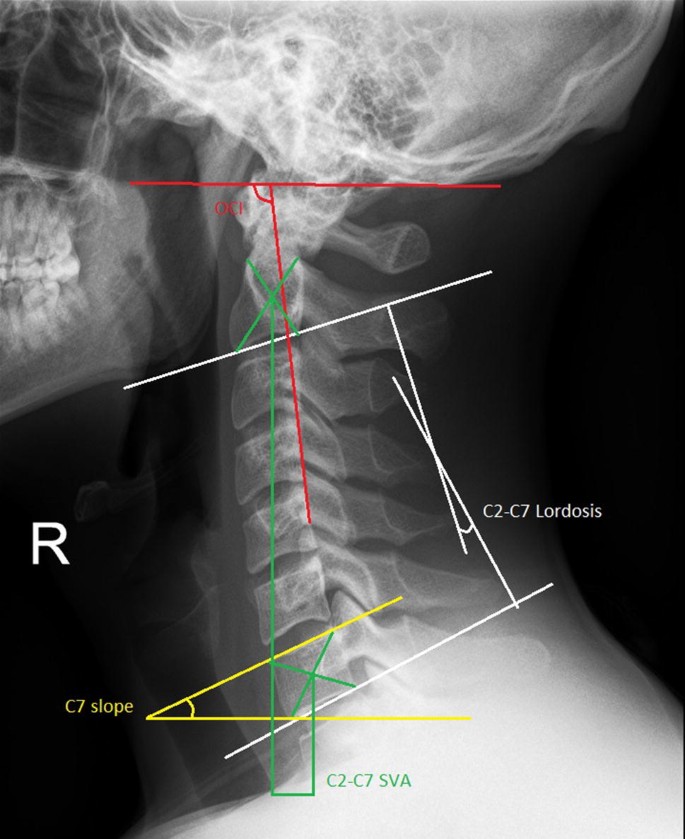
Patients were analysed from two randomized, double-blinded trials comparing anterior cervical discectomy with arthroplasty (ACDA), with intervertebral cage (ACDF) and without intervertebral cage (ACD). C2–C7 lordosis, T1 slope, C2–C7 sagittal vertical axis (SVA) and the occipito-cervical angle (OCI) were determined as cervical sagittal alignment parameters. Radiological ASD was scored by the combination of decrease in disc height and anterior osteophyte formation. Neck disability index (NDI), SF-36 PCS and MCS were evaluated as clinical outcomes.
The cervical sagittal alignment parameters were comparable between the three treatment groups, both at baseline and at 2-year follow-up. Irrespective of surgical method, C2–C7 lordosis was found to increase from 11° to 13°, but the other parameters remained stable during follow-up. Only the OCI was demonstrated to be associated with the presence and positive progression of radiological ASD, both at baseline and at 2-year follow-up. NDI, SF-36 PCS and MCS were demonstrated not to be correlated with cervical sagittal alignment. Likewise, a correlation with the value or change of the OCI was absent.
OCI, an important factor to maintain horizontal gaze, was demonstrated to be associated with radiological ASD, suggesting that the occipito-cervical angle influences accelerated cervical degeneration. Since OCI did not change after surgery, degeneration of the cervical spine may be predicted by the value of OCI.
Dutch Trial Register Number NTR1289.
Trial Register Number ISRCTN41681847.
These slides can be retrieved under Electronic Supplementary Material.
The cervical spine has a crucial role in compensating a distorted global spinal balance. In order to maintain horizontal gaze, the cervical spine will compensate [1]. Regularly, global sagittal imbalance is only present in a very mild form, and subsequently, cervical compensation is only minor. However, even minor cervical spine balance compensation mechanisms may cause accelerated degeneration of the cervical spine segments (ASD). Surgical interventions that possibly interfere with sagittal alignment, like anterior discectomy, may influence ASD, irrespective of the presence of preoperative sagittal imbalance of the whole spine.
In order to quantify cervical spine sagittal alignment, several radiographic parameters have been proposed, including C2–C7 lordosis, C2–C7 sagittal vertical axis (SVA) and T1 slope [2, 3]. It has to be realized though that these parameters also importantly influence each other [4, 5].
Furthermore, occipito-cervical inclination (OCI), defining the occipito-cervical angle, independent of the occipito-cervical distance, is an important sagittal alignment parameter, since it represents the stress on the cervical spine to maintain horizontal gaze [6]. To the best of our knowledge, no study correlated this parameter with cervical ASD previously.
Anterior cervical discectomy and fusion (ACDF) has been a common surgical treatment for cervical radiculopathy since it was initially described in the 1950s [7, 8] and became the gold standard procedure. Recently, artificial disc implantation (ACDA) has been proposed to maintain disc height, restore cervical motion and avoid neck pain and disability in post-surgical follow-up [9]. Limited studies have described the cervical sagittal alignment after ACDA in comparison with ACDF and reported contradictory results. Kim et al. [10] reported that ACDA maintained the cervical sagittal alignment well in comparison with ACDF, but other researchers disputed this advantage and found that the alignment of the cervical spine is unaltered irrespective of the anterior cervical discectomy procedure performed [11, 12]. Most studies, however, only focused on comparing the cervical curvature between ACDF and ACDA, and the other sagittal alignment parameters were rarely investigated.
In the current study, sagittal alignment parameters of the cervical spine are evaluated in patients from two randomized double-blind trials on patients treated by anterior cervical discectomy with or without interbody fusion and arthroplasty for cervical radiculopathy at baseline and a 2-year follow-up. The parameters and the changes in sagittal alignment were correlated with the incidence and progression of radiological ASD and to clinical outcomes.
A prospective, randomized double-blind multicentre trial among patients with cervical radiculopathy due to single-level disc herniation was conducted. Patients were randomly assigned into three groups: anterior cervical discectomy with arthroplasty (ACDA; activ®C, Aesculap AG, Tuttlingen, Germany), anterior cervical discectomy with fusion (ACDF; Cage standalone) and anterior cervical discectomy (ACD). The protocol was approved by medical ethics committees, including an approval for randomization after anaesthetic induction. All patients gave informed consent.
The design and study protocol were published previously [13]. The 2-year follow-up data revealed no differences in clinical outcomes [14].
The trial design was a prospective, double-blind, single-centre randomized study, with a three-arm parallel group. Patients were randomly allocated into three groups: ACDA (Bryan disc prosthesis, Sofamor Danek, Kerkrade, the Netherlands), ACDF (Cage standalone, DePuy Spine, Johnson and Johnson, Amersfoort, the Netherlands) and ACD. The trial was approved by the medical ethics committee. All patients gave informed consent.
The design and study protocol were published previously [15]. The follow-up data up to 8 years post-surgery revealed no differences in clinical outcomes [16].
Lateral X-rays of the cervical spine were obtained with the patients in a standing position and instructed to look straight ahead, with hips and knees extended, in order to obtain a neutral position of the head.
Cervical sagittal alignment parameters were measured preoperatively and 2 years post-operatively (Fig. 1):
The changes of sagittal parameters after surgery, with reference to the baseline values, were investigated as well.
In the ACD group, the disc height decreased from the pre- to the post-operative situation. This might therefore influence the sagittal alignment parameters. Additionally, for this group specifically, the disc height was correlated with the baseline and 2-year follow-up alignment parameters as well.
ASD was defined based on the height of an adjacent level disc and the anterior osteophyte formation on X-rays according to the classification reported by Goffin et al. [18] preoperatively and 24 months post-operatively (Table 1). Since there are no strict criteria to define ASD, evaluation of ASD was performed with three different methods. Firstly, only if neither the superior nor inferior adjacent level demonstrated loss of disc height or anterior osteophyte formation, the patient was graded as ‘non-ASD’; all other patients were graded as ‘ASD’. Secondly, in a separate analysis, ‘mild ASD’ was scored if patients had ‘no’ or ‘minor’ ASD changes in both the superior and inferior adjacent levels, and ‘ASD’ was defined to be present if the classification was ‘moderate’ or ‘severe’ loss of disc height or anterior osteophyte formation in either the superior or inferior level. Thirdly, ASD was evaluated by progression of adjacent level degeneration: ‘ASD progression’ was marked as positive or negative for patients that did or did not increase in Goffin score during follow-up.Table 1 The classification of adjacent segment degenerationFull size table
NDI is a 10-item questionnaire on 3 different aspects: pain intensity, daily work-related activities and non-work-related activities. Each item is scored from 0 to 5, and the total score ranges from 0 (best score) to 50 (worst score). This 50 points score was converted to a percentage (50 points = 100%). The NDI is a modification of the Oswestry Low Back Pain Index and has been shown to be reliable and valid for patients with cervical pathology [19]. The physical-component summary (PCS) and mental-component summary (MCS) are derived from the SF-36 and are summary scores for, respectively, the Physical Quality of Life and the Mental Quality of Life. The PCS and MCS range from 0 to 100, with higher scores representing better self-reported health.
All the data were presented as mean ± standard deviation. Paired t test was used to compare the changes of sagittal alignment parameters between baseline and 2-year follow-up data. Logistic regression analysis was used to determine the correlation between the sagittal balance parameters at baseline with the presence and progression of ASD. Likewise, logistic regression analysis was used to determine the correlation between the changes in sagittal balance parameters during the 2-year follow-up time. Linear regression analysis was used to correlate the disc height and cervical sagittal alignment parameters at baseline and at 2-year follow-up in the ACD group. Linear regression analysis was also performed to correlate the clinical outcome data with the sagittal balance parameters at 2-year follow-up in all groups. The correlations between sagittal alignment parameters were analysed using the Pearson correlation coefficient.
A P value of < 0.05 was considered significant. SPSS software, version 23.0, was used for all statistical analyses (SPSS, Inc., Chicago, IL, USA).
In the current study, 253 patients were included and randomly assigned to ACD (83 patients), ACDF (85 patients) or ACDA (85 patients). At baseline, X-ray data were available for 228 patients and for 168 patients at 2-year follow-up.
Baseline characteristics are presented in Table 2. The mean age of the study population was 45.2 ± 7.3 years, ranging from 27 to 70 years. There was no difference regarding baseline characteristics between treatment groups. Surgery was most frequently at levels C5–C6 and C6–C7.Table 2 Patient demographics by treatment armFull size table
Table 3 demonstrates the characteristics of the cervical sagittal alignment parameters in the different treatment arms. No differences were found regarding sagittal alignment parameters between the three surgical groups neither at baseline nor at 2-year follow-up (P > 0.05). Additionally, it was found that the cervical alignment parameters did not change significantly comparing baseline to post-operative values with the exception of C2–C7 lordosis in the ACDF group (P = 0.048). Irrespective of the surgical method, only C2–C7 lordosis was found to change (increase) significantly over 2 years (from 11.3° to 13.1°, P = 0.023). The other three parameters (OCI, C2–C7 SVA and T1 slope) did not change with a statistical significance. Notably, the angle or slope could be minimally negatively or minimally positively deviating.Table 3 Characteristics of sagittal alignment parameters in subgroupsFull size table
In the ACD group, there was no correlation between the disc height of the target level and cervical sagittal alignment at baseline (P > 0.05). Likewise, this correlation was absent at 2-year follow-up (P > 0.05). There was a decrease in disc height, but this did not impact overall balance.
Preoperatively, the incidence of ASD did not differ in the three groups: 38% in the ACD group (27 patients), 36% (29 patients) in the ACDF group and 29% (22 patients) in the ACDA group (P = 0.428). At 2-year follow-up, ASD increased to 63% of patients in the ACD group (35 patients), and 55% (28 patients) in the ACDF group and to 56% (34 patients) in the ACDA group. Likewise, between three groups, there was no statistically significant difference (P = 0.674).
If ASD was considered to be scored as ‘ASD’ only if disc degeneration and/or the presence of osteophytes was moderate or severe, the incidence of ASD was still comparable in the three treatment arms at baseline: 16% in the ACD group, 14% in the ACDA group and 13% in the ACDA group (P = 0.905). And likewise, 2 years after surgery, the incidence of ASD did not differ between three groups (29% in the ACD group, 26% in the ACDF group and 20% in the ACDA group; P = 0.522).
Furthermore, the progression of ASD was also investigated, comparing follow-up to baseline data. At 2 years after surgery, the proportion of positive ASD progression was comparable in the three treatment arms (33% in the ACD group, 25% in the ACDF group and 31% in the ACDA group; P = 0.693).
In order to study the relationship between cervical sagittal alignment parameters and ASD, subjects were dichotomized according to the presence and progression of radiological ASD, irrespective of the surgical method. The average values of sagittal alignment parameters of subjects with and without ASD are shown in Table 4.Table 4 Cervical sagittal alignment parameters with the presence and progression of ASDFull size table
At baseline, a higher OCI value was significantly correlated with the presence of ASD (OR 1.05; 95% CI 1.01–1.09; P = 0.009). If patients were dichotomized into mild ASD and ASD, the result was similar (OR 1.05; 95% CI 1.00–1.11; P = 0.044). C2–C7 lordosis, C2–C7 SVA and T1 slope failed to show a correlation with ASD (Table 5).Table 5 Factors associated with the presence of ASD at baselineFull size table
At 2-year follow-up, again, OCI with higher value was correlated with the presence of ASD (OR 1.08; 95% CI 1.04–1.13; P < 0.001). If patients were dichotomized into mild ASD and ASD, the correlation between higher OCI and ASD was detected as well (OR 1.11; 95% CI 1.06–1.16; P < 0.001). Patients with higher OCI value were likewise correlated with the positive progression of ASD (OR 1.05; 95% CI 1.01–1.09; P = 0.023) (Table 6).Table 6 Factors associated with the presence and progression of ASD at 2-year follow-upFull size table
As stated above, no significant changes in mean OCI values existed between baseline and 2-year follow-up. On an individual level, changes were small for the vast majority of patients, but considerate for a minority of patients (Fig. 2). However, no correlation was demonstrated between the change in OCI value and the progression of ASD. Neither was there a correlation between the change in sagittal balance parameter and progression of ASD for the other parameters (Table 7).
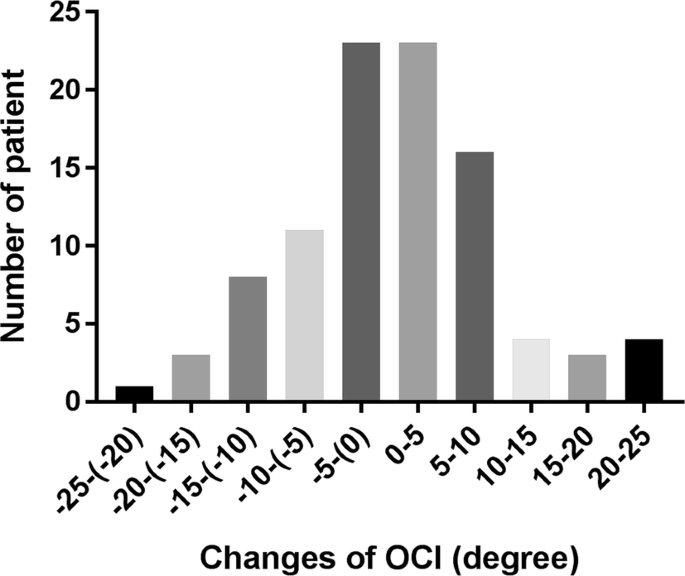
Table 7 The change of sagittal alignment parameter associated with progression of ASD at 2-year follow-upFull size table
The clinical outcomes represented by NDI, PCS and MCS were comparable between the three treatment groups, both at baseline and at 2-year follow-up (Table 8). Therefore, the clinical outcomes were studied irrespective of surgical methods. At baseline, the mean NDI was 39.7 ± 15.4, mean PCS was 43.3 ± 13.5, and mean MCS was 59.1 ± 21.5. At 2 years after surgery, the NDI decreased to 16.4 ± 17.1. PCS and MCS increased to 73.9 ± 23.6 and 77.6 ± 21.8, respectively.Table 8 Characteristics of clinical outcomeFull size table
At 2-year follow-up, the values of C2–C7 lordosis, C2–C7 SVA, OCI and T1 slope failed to correlate with clinical conditions, and neither was there a correlation of clinical outcome to the changes of these parameters (P > 0.05).
SVA was significantly correlated with T1 slope (0.45–0.54, P < 0.01) and OCI (0.20–0.37, P < 0.01). C2–C7 lordosis was correlated with T1 slope as well (0.40–0.55, P < 0.01) (Table 9).Table 9 Correlation between sagittal alignment parametersFull size table
Cervical sagittal alignment was demonstrated not to be affected by anterior discectomy during 2-year follow-up after surgery. The alleged superiority of maintaining cervical alignment in arthroplasty was not established. The occipito-cervical angle, being crucial in maintaining horizontal gaze, was identified as an important factor associated with radiological adjacent segment degeneration.
OCI is a relatively new radiological parameter of the angle between the occiput and the cervical spine proposed by Yoon et al. [6]. In this study, it is first applied to investigate the relationship with radiological ASD and clinical outcomes in patients with cervical disc degeneration. Wu et al. [20] reported before that the occipito-C2 angle was correlated with post-operative ASD in a patient group that underwent occipitoaxial spondylodesis. Theoretically, the occipito-cervical angle is dictated by horizontal gaze, and if this angle is imbalanced, it may well lead to compensation of subaxial cervical curvature, which will eventually lead to accelerated degeneration of the cervical spine [21]. This could explain the strong correlation of OCI with ASD detected in this study.
Remarkably, the OCI angle did not change after surgery, although there was significantly more ASD in patients with a higher OCI. Therefore, the result of this study suggests that accelerated degeneration of the cervical spine is dictated by the OCI angle. Thus, accelerated degeneration of the cervical (subaxial) spine can be predicted if the OCI is known. Ideally, a cut-off point of the OCI would be available. ASD is determined in this study in three ways, and therefore, three different values are available: for non-ASD, an angle of 102°–104° was measured, and for ASD angles, varying between 108° and 113° were observed (Table 4). Future studies are needed to confirm and determine cut-off values. Moreover, long-term follow-up studies are needed to study whether ASD or subaxial degeneration continues during longer follow-up or that it stabilizes.
In the current study, no correlation between clinical outcome and sagittal balance parameters could be demonstrated. The C2–C7 SVA and T1 slope did not change in follow-up of surgery, the C2–C7 lordosis only increased minimally, and they did not demonstrate a correlation with ASD. Therefore, an absence of correlation with the clinical outcome is not surprising. However, previous studies did demonstrate an association between sagittal alignment parameters to the quality of life [1, 22]. Tang et al. [23] found that the C2–C7 SVA was negatively correlated with PCS and positively correlated with NDI scores after multilevel cervical posterior fusion. Hyun et al. [24] found that C2–C7 SVA greater than 43.5 mm was corresponded to severe NDI (> 25). Nevertheless, Jeon et al. [3] and Kwon et al. [25], which compared similar radiographic parameters with NDI and visual analog scale (VAS), reported that no cervical sagittal alignment parameters were significantly correlated with clinical outcomes after ACDF surgery with 3 levels and 2 levels, respectively, which are consistent with our results. It has to be noted though that these authors describe different surgical approaches. Tang et al. [23] and Hyun et al. [24] reported on patients with posterior cervical fusion surgery. Jeon et al. [3] and Kwon et al. [25] reported on multilevel anterior fusion surgery of the cervical spine and demonstrated threshold values for C2–C7 SVA of 40 mm [23] and 43.5 mm [24] in contrast to the values that we reported in the majority of patients (mean value 20.6–22.5 mm).
A limitation of this study is that we have analysed radiographic parameters with a follow-up of only 2 years after surgery. In contrast to our results, other research groups did demonstrate a lower occurrence of ASD in ACDA compared with ACDF with longer follow-up periods [26,27,28,29,30]. These articles, however, had a high or intermediate risk of bias, and estimates of effect were not sufficiently described. Therefore, the level of evidence that ASD occurs more often in ACDF than in ACDA is low [31]. Moreover, a recent study with low risk of bias demonstrated that the presence of both clinical ASD and radiological ASD was similar in the ACDA and ACDF at 5-year follow-up [32]. It is thus debatable whether ASD will demonstrate differences between the three groups upon longer follow-up periods. However, in our opinion, the current data on ASD, demonstrating a gradual increase in ASD in all three groups, make this rather unlikely.
The choice of the intervertebral device in anterior cervical discectomy surgery does not influence cervical sagittal alignment. OCI was demonstrated to be an important factor associated with radiological ASD, suggesting that occipito-cervical alignment influences accelerated cervical degeneration. The correlation between cervical sagittal alignment parameters and clinical outcome is absent.
This work was supported by China Scholarship Council and the Department of Neurosurgery, Leiden University Medical Centre. Xiaoyu Yang received support from both funding agencies. The NECK trial was sponsored by B. Braun Medical and the Department of Neurosurgery, Leiden University Medical Centre, The Netherlands.
Correspondence to Xiaoyu Yang.
There is no conflict of interest for the current study.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Below is the link to the electronic supplementary material.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.

C/ San Pedro de Mezonzo nº 39-41
15701 – Santiago de Compostela
Teléfono: +34 986 417 374
Email: secretaria@sogacot.org
Coordinador del Portal y Responsable de Contenidos: Dr. Alejandro González- Carreró Sixto