Gabriel Liu, MB BCh, BAO, MSc, FRCSI, FRCSEd (Ortho), FAMS; Muhammed Y. Hasan, MBBS, MRCS (Edin); Hee-Kit Wong, MBBS, MMed (Surg), FRCS, MCh (Orth), FAMS
Spine. 2018;43(2):E68-E74.
Study Design. Case-series.
Objective. To report our modified iliac-screw insertion technique and its clinical outcomes.
Summary of Background Data. Iliac-screws are one of the preferred methods for modern spinopelvic-fixation. However, the technique is not without complications, predominantly because of iliac-screw head prominence, leading to pain and revisions. Conventional iliac-screw entry point is sited superficially at the posterior-superior-iliac-spine (PSIS) contributing to screw-head prominence. We propose a more low-profile, subcrestal entry point that is more medial and inferior to the PSIS at the medial wall of the iliac crest, lying underneath the crest but above the sacroiliac joint. This position keeps the screw-head low profile and in-line with proximal instrumentation to ease rod engagement.
Methods. Ten consecutive patients who underwent spinal deformity correction surgery using the modified iliac-screw entry point fixations were enrolled. Clinical, radiological, and surgical parameters were reviewed.
Results. Five males and five females with average age of 66 years and average follow up of 29 months were reviewed. Mean preoperative Cobb angle and C7-SVA were 32.1° and 10.3 cm, respectively. Surgical indication was progressive deformity and neurogenic claudication in eight cases and fracture in two cases. Twenty noncannulated, polyaxial iliac-screws with median dimension of 7.5 x 75 mm were inserted free hand. Bilateral S1 screws were used in all except two cases. Only five out of 16 iliac-screws with concomitant S1 screws needed side-connectors. At the last follow up only one iliac-screw head was felt to be prominent but without pain in a Parkinson's patient. None of the 10 patients had cases of revision, breakages, or sacroiliac pain.
Conclusion. Subcrestal iliac-screw insertion is feasible, safe, and has the potential to reduce screw-head complications and avoid the use of side-connectors, lowering construct complexity and cost. The technique has the advantage of both the low-profile S2 alar iliac screw and the ease of free-hand insertion of the traditional iliac-screw.
Level of Evidence: 4
Pelvic fixation utilizes the anatomical advantage of the human pelvis to add strength and stability to spinal constructs. Pelvic anchoring has been shown to reduce implant failure and promote arthrodesis at the lumbosacral junction.[1] The technique is used widely across a spectrum of spinal surgeries including deformity correction, lumbosacral trauma, and spinal metastatic disease.[1–3]
In the last decade, pelvic fixation via iliac-screws fixation has gained popularity in spinal deformity correction surgery, where its usage has shown to reduce pseudoarthrosis, protect failure of lumbosacral implants, and prevent sacral fractures at lumbosacral junction.[1,4,5] Biomechanically iliac-screws offer a more stable fixation when compared with other fixation modalities such as Galveston rods, sacral screws, Cotrel-Dubousset Chopin, and butterfly plate.[6] Iliac-screws lie lateral to the proximal construct in the coronal plane allowing better resistance against distal implant pullout, whereas in the sagittal plane fixation extends anterior to the spine creating a moment arm ventral to the spinal axis to better maintain sagittal deformity correction.[6]
Fixations with conventional iliac-screws have some drawbacks primarily because of its screw head prominence and the subsequent need for implant revisions.[1,4] The conventional entry points described in literature were generally cited at the posterior superior iliac spine,[4,5] which is close to the skin and often causes postoperative gluteal pain from the prominent screw head. Reported incidence of screw revision because of prominence and pain varies from 6% to 34%.[4,5,7] Furthermore this entry point at the posterior superior iliac spine (PSIS) on the ilium makes it difficult to engage the rods to the screws. A side-connector linking the iliac-screw and cephalic instrumentation is required.[5] Recent use of S2 alar iliac-screws (S2AI) reduces some of the complication related to the conventional iliac-screws. However, the use of S2AI screw violates the sacroiliac (SI) joint[8,9] and often requires intraoperative fluoroscopy to guide accurate screw insertion.
The aim of this article is to report the use of free hand, low profile, subcrestal iliac-screw as an alternate to conventional iliac-screw. The subcrestal screw is inserted at medial wall of the iliac crest, underneath the crest and above the SI joint. This low profile subcrestal screw avoids SI joint violation, reduces screws head profile and keeps the screw head in line with the proximal instrumentation to ease rod engaging and reduce implant related complications.
Ten consecutive patients underwent the free hand, low profile, subcrestal iliac screw insertion from 2010 to 2016 by a single surgeon (G.L.). Patient's clinical, surgical, and radiological data was collected with attention to document iliac screw related surgical complications. Our modified technique of iliac screw entry point is described below.
After exposing the lumbosacral spine, subperiosteal dissection is performed to expose the inner table of iliac crest to see the PSIS. Less soft tissue dissection is required in this technique modification as there is no need to expose the entire iliac crest with both inner and outer tables. The subcrestal iliac screw entry point is location 2 to 3 cm caudal to PSIS just below S1 sacral foramen (Figure 1A and Figure 1B). This point lies 1.5 to 2 cm beneath the iliac crest and above the SI joint allowing screw head to be concealed under the medial ridge of the crest reducing prominence related complications (Figure 2). The entire iliac crest is preserved in this technique modification as opposed to the conventional technique in which a wedge is osteotomized from out of PSIS to house the conventional iliac screw.
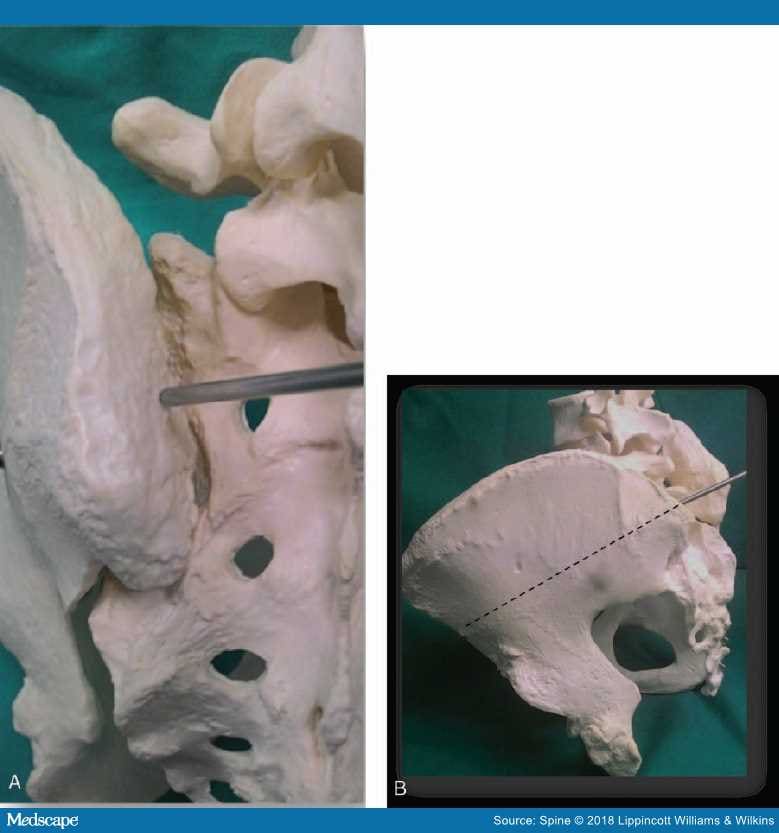
The subcrestal iliac screw entry point is location 2 to 3cm caudal to PSIS. This point lies 1.5 to 2cm underneath the iliac crest and above the SI joint allowing screw head to be concealed (A). The trajectory is 458 caudally and laterally towards the anterior inferior iliac spine (dotted line) (B).
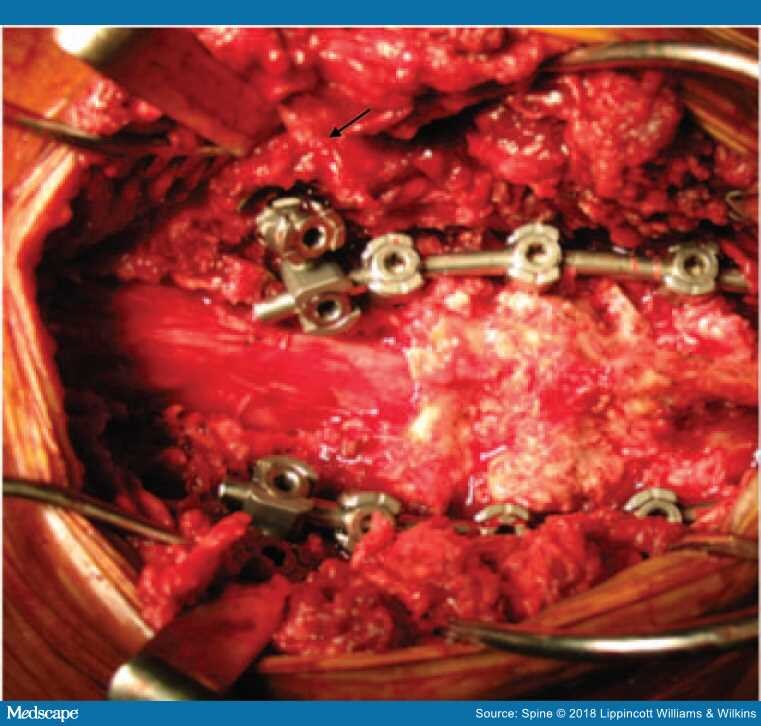
Figure 2.
Iliac screw head lie under the medial iliac crest ridge (arrow) reducing prominence. In this this case a side connector was used to connect iliac screw to S1 screws.
The screw is then inserted using free hand technique without fluoroscopic guidance. A ball tip burr is used to create a pilot hole at the entry point. A straight long awl is used to deepen the pilot hole. The screw trajectory is planned similar to the conventional iliac screw technique in which screw is aimed towards the AIIS (anterior inferior iliac spine) or greater trochanter 35 to 45 degrees cephalocaudal and mediolaterally (Figure 1B).
Each subcrestal iliac screw trajectory is fine tuned by following approximately the inclination parallel to the medial wall of the iliac crest and the tactile feeling of the crunching soft cancellous bone at the awl tip between the hard outer and inner cortical table of the iliac crest. Centrally placed awl in ilium is confirmed by the teardrop ilium radiological view to confirm correct screw position. A long guide wire is used as a feeler to check the breeches and the integrity of the screw track. The screw track is then under-tapped by one size to the desired screw diameter. Screw length was aimed to be more than 75 mm with screw tip anterior to the lumbar spine. We current prefer to use a fully threaded polyaxial screws with diameter size 8 mm and above. The S1 screw is then planned and placed in-line with respect to the subcrestal iliac screw position for easy screw-rod attachment.
Another technical step we found beneficial was the use of minimally invasive (MIS) tubular sleeve connected to the noncannulated iliac screws and used as a reduction device for easy iliac screw-rod engagement. The rod is engaged using cantilever reduction in caudal to cephalad direction (Figure 3A).
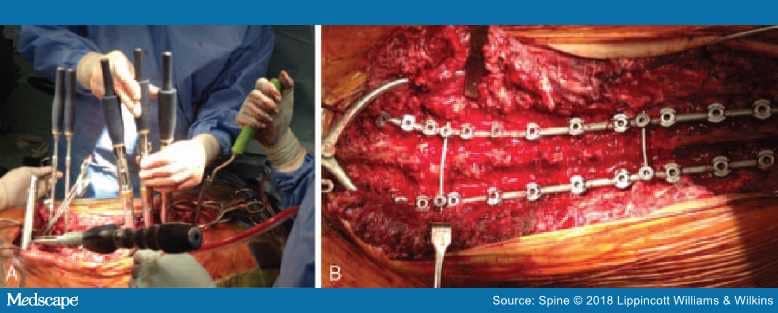
Figure 3.
Using MIS sleeve and screw extension for rod insertion (A). This avoids the use of side-connectors in the presence of concomitant S1 screw as shown below (B).
Five females and five male consecutive patients who had open subcrestal iliac-screw insertion were reviewed. The mean adult age was 66 years (55–75 yrs). Mean preoperative Cobb angle and C7-SVA were 32.1° (2–82°) and 10.3 cm (2–16.3 cm) respectively. Preoperative median back and leg VAS score was 8 (7–10). Indication for surgery was symptomatic progressive deformity and neurogenic claudication in eight cases and vertebral fracture in two cases (Table 1).
Twenty noncannulated full threaded polyaxial iliac-screws using this new technique modification were insertion successfully using free hand. Median iliac screw diameter and length were 7.5 mm (7.0–8.0 mm) and 75 mm (65–75 mm), respectively. Bilateral S1 screws were used in all except two cases. Only five out of 16 (31%) iliac screws with concomitant S1 screws needed side-connectors linking iliac screws to the rod (Table 2). This occurred in early cases as subsequently the need for using side-connectors reduced with the use of long MIS screw sleeve attached to iliac-screw which acted as a reduction device for iliac-screw-rod engagement (Figure 3A and Figure 3B). Mean postoperative scoliosis Cobb angle was reduced to 8.5 (2–25) degrees with mean C7-SVA of 4.7 cm (2–9 cm) (Table 3).
Mean patient follow-up of 29 months (6–60 months). Patient A developed proximal junctional fracture at T7 2-months after surgery, requiring a vertebroplasty. Patient C developed proximal segment osteolysis (T11–12) 6-months postsurgery requiring extension of proximal instrumentation and fusion till T3. With regards to iliac-screw specific complications, there was only one case of implant prominence in a patient with Parkinson's disease (Patient E); however, at the last follow up at 4 years there was no screw site pain nor wound issues and the screw was not revised (Table 3). Overall there were no postoperative SI joint symptoms, screw loosening, breakage, or iliac-screw revisions in the current study.
Spinopelvic fixation via iliac-screw placement is one of the current preferred techniques in achieving a stable lumbosacral construct during surgical management of adult spinal deformity.[1]In vitro biomechanical comparison between historical lumbopelvic fixation techniques found iliac screw to be the most superior method for protecting sacral screw breakage and spinopelvic construct failures.[6,10,11] Clinical advantages of iliac-screw fixation have been well described in deformity correction surgery. In a 5-year follow up on 67 patients who underwent lumbosacral fusion with bilateral sacral and iliac screws, Tuschiya et al[4] demonstrated a fusion rate of 92.5%. Kasten et al[5] followed 78 patients with iliac screws for at least 2 years and noted a fusion rate of 84.7% with only 6.3% of pseudoarthrosis occurred at the LSJ. Both these studies reported no sacral screw failures, sacral fractures nor SI joint arthritic changes.
Despite favorable LSJ fusion rates and protective impact on sacral implants, conventional iliac screw fixation is associated with complications. The technique requires extensive surgical dissection to expose both inner and outer table for screw insertion, which adds to blood loss and infection risk. A major concern of conventional iliac screw technique is buttock pain because of screw head prominence, which results in a high screw removal rates.[12–14]
Iliac-screw head prominence has been attributed to the relatively superficial iliac-screw entry point. Conventional screw entry is located at top of the surgically wedged iliac-crest to countersink the screw head. Despite this maneuver the conventional screw is still prominent and prone to gluteal pain and wound dehiscence. A recent alternative method of spinopelvic fixation is the S2 alar iliac (S2AI) approach. In this approach, the screws are placed on the lamina between the S1 and S2 foramen.[15,16] Because of the S2AI screw's deeper and medialized entry point away from the ilium, S2A1 screws are more low-profile and avoid implant prominence compared with the classical iliac screw techniques. Recent comparisons with conventional iliac screws do indicate a lower rate of implant related complications.[14,17,18]However, the screw trajectory of S2AI screw traverses across the SI joint[8,9]and may have potentially unknown long-term complications.
Our reported subcrestal iliac-screw modification places the iliac-screw entry point in the medial wall or the inner table of the ilium below the iliac-crest but above the SI joint. This design intended to conceal the iliac-screw head to be placed underneath and to be protected by the iliac crest, hence avoids post insertion screw head prominence and its related complications. As the screw entry point location is at the medial wall beneath the ilium, there is no need to dissect out the entire ilium required for the conventional iliac-screw entry. This resulted in less dissection, tissue damage, blood loss, and faster surgery with possible better wound healing. Because of the more medially placed screw entry point and the use of MIS screw sleeve as a reduction device we were able to engage the rod to the iliac-screw head without the use of iliac-screw side-connector (Figure 3A, Figure 3B and Figure 4). This new entry point made the subcrestal iliac-screw more in-line with the proximal construct and hence made the iliac-screw-rod engagement relatively easy. Omitting the side-connector significantly reduced the cost of surgery, as each connector is priced higher than the cost of the iliac-screw. Furthermore the subcrestal iliac-screw entry point does not require a wedge to be cut out from the iliac-crest, resulting in a lesser chance of iatrogenic iliac crest fracture and postoperative iliac and gluteal region pain.

Figure 4.
Patient B with degenerative scoliosis and multilevel lumbar stenosis underwent T9-iliac PSF along with TLIF L4–5, L5-S1, and decompression L2–3. No side-connectors were used for iliac screw rod linkage.
The subcrestal iliac screw has the advantage of not penetrating the SI joint when compared to S2AI screw avoiding potential iatrogenic SI joint damage and pain. Another potential disadvantage in the case of S2A1 screw was that it is inserted through multiple cortical joint surfaces from sacrum to SI joint may potentially contribute to the higher fatigue stress at screw-head interface. Guler et al[19] in a study on lumbosacral fixations noted that in cases with suboptimal sagittal plane correction, S2AI polyaxial screws seem to have higher risk of short-term acute failure compared to iliac wing screws. Enercan et al[20] observed 33.6% S2AI screw loosening in severely osteoporotic patients and reported that failure may be attributed to the fact that the proximal one-third of screw fixation shaft is located in osteoporotic sacral alar bone. Lastly, passage of S2AI screw through multiple cortical joint surfaces from sacrum often requires fluoroscopic guidance to ensure correct placement. This constant fluoroscopic guidance is not required in the free hand, subcrestal approach, and hence reducing radiation exposure and potentially allows a faster ilium fixation when compared to S2AI screw.
One of the limitations of our report is the small sample size. We also routinely do not perform postoperative CT scans, though some patients in our cohort did have CT imaging to check for fusion and did not show any iliac-screw SI joint violations. Overall it has been shown in the current study that the subcrestal iliac-screw was stable and without complications over a 1 to 5 year follow-up period. A larger series including comparison with conventional iliac screw and S2AI techniques is recommended to further elicit its long-term benefit and safety.
Free hand, in-line, low profile, subcrestal iliac-screw is safe, easy, and reproducible technique. It reduces the incidence of postoperative prominent screw head related complications and avoids the use of side-connectors to reduce construct complexity and cost. It has the advantage of both the low profile S2AI screw and the ease of free hand, fluoroscopy free insertion benefit of the traditional iliac screw.
REFERENCES
Comments