To investigate whether the World Health Organization Safety Surgical Checklist (SSC) is an effective tool to reduce complications in spinal surgery.
We retrospectively evaluated the clinical and radiological charts prospectively collected from patients who underwent a spinal surgery procedure from January 2010 to December 2012. The aim of this study was to compare the incidence of complications between two periods, from January to December 2010 (without checklist) and from January 2011 and December 2012 (with checklist), in order to assess the checklist’s effectiveness.
The sample size was 917 patients with an average of 30-month follow-up. The mean age was 52.88 years. The majority of procedures were performed for oncological diseases (54.4%) and degenerative diseases (39.8%). In total, 159 complications were detected (17.3%). The overall incidence of complications for trauma, infectious pathology, oncology, and degenerative disease was 22.2%, 19.2%, 18.4%, and 15.3%, respectively. No correlation was observed between the type of pathology and the complication incidence. We observed a reduction in the overall incidence of complications following the introduction of the SSC: In 2010 without checklist, the incidence of complications was 24.2%, while in 2011 and 2012, following the checklist introduction, the incidence of complications was 16.7% and 11.7%, respectively (mean 14.2%).
The SSC seems to be an effective tool to reduce complications in spinal surgery. We propose to extend the use of checklist system also to the preoperative and postoperative phases in order to further reduce the incidence of complications.
These slides can be retrieved under Electronic Supplementary Material.
The definition of complication in spinal surgery is currently not clear. It varies greatly both in different literature reports and between different surgical specialties [1,2,3,4,5,6]. Dindo and Clavien [4] defined a surgical complication as “any deviation from the ideal postoperative course that is not inherent to the procedure and does not comprise a failure to cure.” Unfortunately, this definition is not universally adopted. The literature has different definitions, classifications, severity scales, and methods of identifications and reporting of surgical complications, making their comparison difficult [3].
In general, the complication rate after spinal surgery ranges between 7 and 20% [1, 2, 7,8,9,10,11], while orthopedic surgery generally has a mean rate of complications of 5% [12].
Prospective studies reported a higher incidence of complications compared with that in retrospective studies, due to more accurate record-keeping, the absence of recall bias, and clear definitions of complications [2, 7]. The rate of complications in spinal surgery does not appear to be lowered within the last 10 years, despite the well-known risk factors reported in the literature [9, 10, 12,13,14,15,16,17].
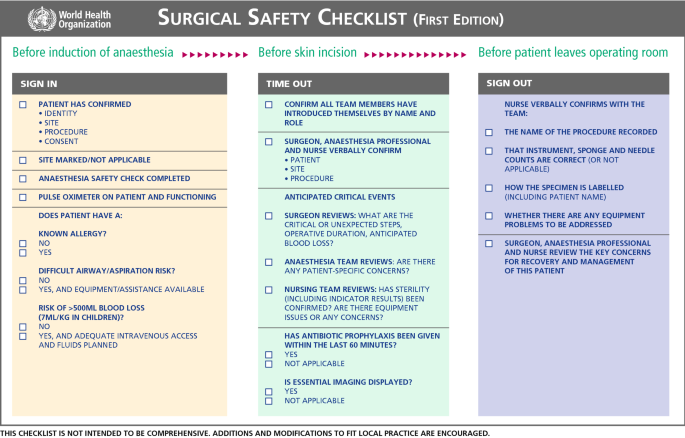
To face the problem of surgical complications, which is generally relevant in the surgical fields, an intraoperative checklist (Safety Surgical Checklist) was elaborated and released by the World Health Organization in 2008, and its use has been described in 2009 [18]. In our institution, the WHO Surgical Checklist was introduced in 2011.
In spinal surgery, many preventive measures were investigated to reduce complications [19,20,21,22,23,24], but there is no report on the effectiveness of the WHO checklist in reducing complications.
The aim of this study was to compare the incidence of the complications between the two periods, from January to December 2010 (without checklist) and from January 2011 and December 2012 (with checklist), in order to assess the checklist’s effectiveness.
A retrospective and single center study was carried out of patients who underwent spinal surgery during the 3-year period from January 2010 to December 2012. The study was approved by the local ethics committee. All patients at the time of admission were asked to sign an informed consent to prospectively collect demographic, surgical, clinical, and quality-of-life information for research purposes.
The inclusion criteria were surgical patients with degenerative, traumatic, infectious (hematogenous spondylodiscitis), and oncological spinal diseases, consented to participate in the study by signing the consent form. Patients with surgical site infections secondary to previous surgery were excluded from the study.
Patients were classified according to the spine pathology and the different presentation of the complication.
According to the pathology treated, there were oncological, degenerative, traumatic, and infectious groups.
Complications were divided into seven categories:
The complications’ classification and the patients’ inclusion into the categories were performed by independent investigators, i.e., non-MD clinical researchers (1 research nurse and 1 clinical research assistant) not directly involved in the care of the patients. This was done to avoid the bias to which surgeons could be exposed in assessing the patients they had themselves operated on.
An intraoperative checklist (Safety Surgical Checklist), elaborated by the World Health Organization (WHO) in 2008, was introduced for the first time in our center in 2011.
The intraoperative checklist starts 1 h before the skin incision and finishes at the end of the surgery. It is composed of 19 items, performed before induction of anesthesia, before skin incision, and before the patient leaves the operating room (Fig. 1). These items allow the surgeons and the medical staff to be aware of different critical points.
We registered the complications arising from 2010 to 2012, assessing the possible differences before and after the checklist’s introduction.
Statistical analyses were conducted with SPSS v21.0 (SPSS Inc., Chicago, Illinois). Mean values and standard deviations (SD) were calculated for continuous variables, which were compared between groups by using heteroscedastic two-tailed Student’s t tests. Categorical variables were analyzed using a Pearson’s two-tailed Chi-squared test. A p value < 0.05 was considered statistically significant.
The sample size studied was 917 patients with a mean follow-up time of 30 months, ranging from 12 to 48 months. The mean age was 52.9 years old, ranging from 3 to 93 years, with similar distribution by gender. The majority of procedures were performed for oncological pathologies (499; 54.5%) and degenerative diseases (363; 39.7%). Table 1 summarizes patients’ demographic data. Patients treated in 2010 without the use of the WHO checklist were 285, while patients treated in 2011 and 2012 with the use of WHO checklist were 632.Table 1 General demographics and diagnosis of the study populationFull size table
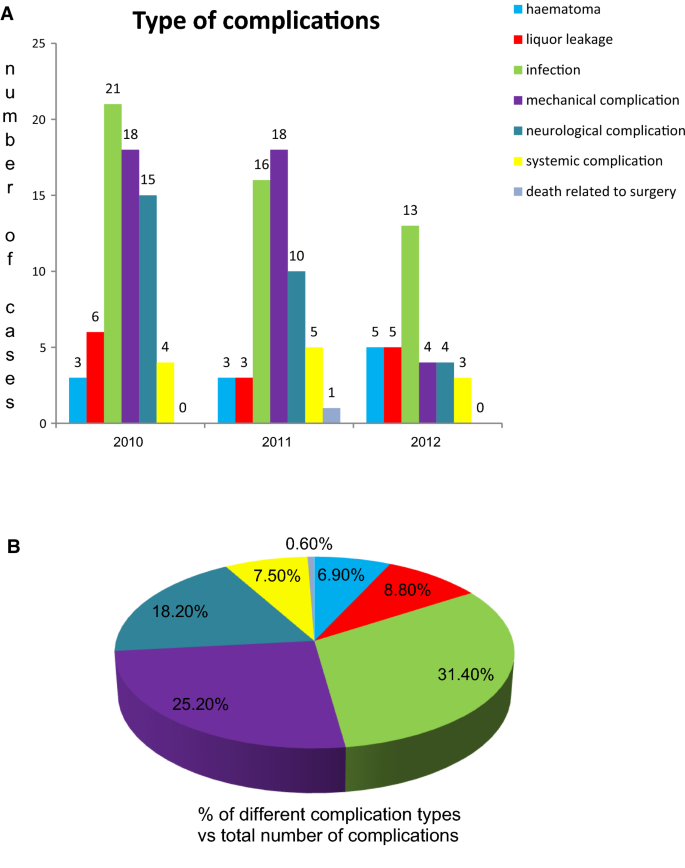
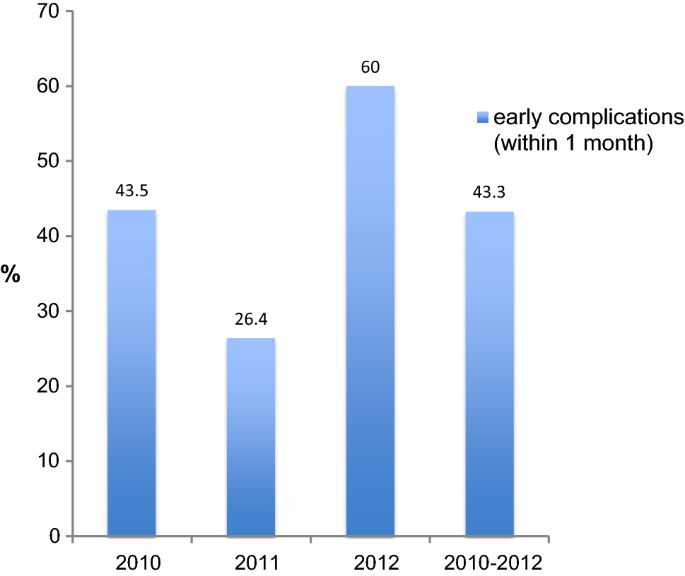
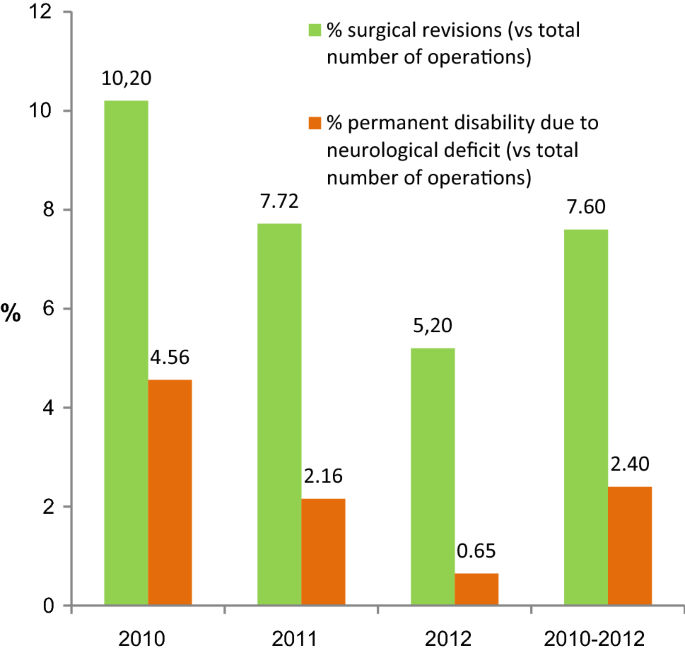
There were complications in 107 patients (11.6%) over 917 spinal surgery procedures performed, with 159 (17.3%) complications overall. The incidence of overall complications for trauma, infectious pathology, oncology, and degenerative disease was 22.2%, 19.2, 18.4%, and 15.3%, respectively. No correlation was observed between the type of pathology and the incidence of complications (p = 0.48). The most frequent complications were wound infection (5.5%), mechanical complications (4.4%), and neurological injury (3.2%). Considering that almost 95% of the patients analyzed were affected by oncologic and degenerative diseases [864 patients (94.22%) vs. 53 patients (5.78%) affected by traumatic and infectious diseases], we compared the incidence of complications in these two groups, observing a trend to a higher wound infection complications (7.4%) in oncologic patients, while a trend to a higher rate of mechanical complications (5.8%) was observed in patients with degenerative diseases, even in the absence of statistical difference (p = 0.12). The incidence of complications according to diagnosis and operation period is summarized in Table 2 and represented in Figs. 2 and 3. In the period analyzed, early complications (arising within 1 month after surgery) were 43.3% globally of all complications (Fig. 4). Moreover, 7.6% of 917 interventions required a surgical revision due to postoperative complications and 2.4% of 917 interventions had neurological sequelae involving permanent damage (Fig. 5).Table 2 Incidence of complications according to diagnosis and operation periodsFull size table
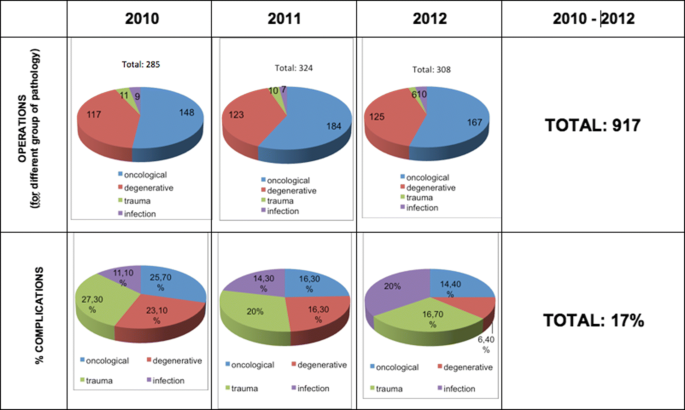
We observed a reduction in the overall incidence of complications following the introduction of the WHO Safety Surgical Checklist: In 2010, the incidence of complications was 24.2% without the checklist, while in 2011 and 2012, following the introduction of the checklist, the incidence of complications was 16.7% and 11.7%, respectively (mean 14.2%) (p < 0.0005).
Spinal surgery complications are still a relevant and unsolved problem. The incidence of complications in spinal surgery literature ranges between 7 and 20% [1, 2, 7,8,9,10,11]. The purpose of this study is to investigate whether the World Health Organization (WHO) Safety Surgical Checklist is an effective tool to reduce complications in spine surgery. In our study population, a reduction in the overall incidence of complications has been observed following the introduction of the WHO Safety Surgical Checklist: In 2010, without the use of the checklist, the incidence of complications was 24.2%, while in 2011 and 2012, following the checklist introduction, the incidence of complications was 16.7% and 11.7%, respectively (mean 14.2%) (p < 0.0005).
We faced two aspects of spinal surgery complications: (1) the collection and classification; (2) the use of preventive measures to improve safety.
Nasser et al. [7] performed a systematic evidence-based review of 105 published studies concerning spinal surgery (84 retrospective, 21 prospective) and found a higher incidence of complications (19.9%) in prospective studies compared with retrospective studies (16.1%). This is secondary to the greater accuracy of record-keeping, the absence of recall bias, and clear definition of complication [2, 7, 17]. The incidence of complications varied widely in spinal surgery literature, even in prospective studies. Rampersaud et al. [3] reported an overall incidence of intraoperative adverse events of 14% (98 adverse events in 700 patients), but only 23 adverse events led to postoperative clinical sequelae for an overall intraoperative complication incidence of 3.2%, while Yadla et al. [2] reported a very high rate of early complications (those occurring within 30 days of surgery): global incidence of 53.2%, with a minor complication incidence of 46.4% and a major complication incidence of 21.3%.
There is no standard definition of complications in spine surgery literature [3]. Different definitions and classifications of complications by different investigators make difficult to compare studies. The Clavien–Dindo and SAVES capture and grading systems [25,26,27] divide the severity of surgical complications into levels based on the grade of treatment required to face the complication. Complications were categorized as major or minor by Glassman et al. Significant complications requiring reoperation or leading to permanent deficit were considered major complications. Other general medical adverse events or perioperative events with time-limited effect were considered minor complications [28].
To date, few studies have evaluated the effect of complication severity on clinical outcomes [28,29,30]. Glassman et al. analyzed a prospective multicenter database for adult spinal deformity to explore the effects of major and minor complications on 1-year disability, pain, postoperative quality of life and found that major complications, although rare, evidently deteriorated the quality of life [28]. Fritzell et al. [29] found no significant differences of effects of major and minor complications on 2-years outcomes in three different types of fusion surgery. Grainger et al. explored the relationship between severity of complications and outcomes in a larger sample of patients following Clavien–Dindo classification of complications and found that the severity of perioperative surgical complications does not appear to influence 1- or 2-year pain and disability outcomes [30]. Lambat et al. confirmed, through a large retrospective study, that Oswestry Disability Index (ODI) at 2-year follow-up was not statistically different between patients having no complications, minor complications, or major complications. However, if the minimum clinically important difference (MCID) for ODI was analyzed, it resulted statistically significantly smaller in the major complication group (31%) than in the minor complication (51%) and no complication groups (65%; p < 0.001) [10], demonstrating an impact of complications on outcome.
Chen et al. recently conducted an interesting experiment. They compared the complications rate among groups of patients undergoing spine, hip, knee, and shoulder surgery; the study was a 10-week prospective study where SAVES V2 and OrthoSAVES were used by six orthopedic surgeons and two independent, non-MD clinical reviewers to record adverse events after all elective procedures. For a spine surgeon, the first important result of this study was the highest rate of complications in the spinal surgery group compared to the other surgeries, but the most important observation of this study was that overall, 99 adverse events were captured by the reviewers, compared with 14 captured by the surgeons (p < 0.001); surgeons adequately captured major adverse events, but failed to record minor events that were captured by the reviewers; in the spinal surgery group, reviewers captured 45 adverse events versus 8 captured by surgeons [31].
The study by Chen et al. [31] confirmed the rate of complications as a problem to be urgently faced in spinal surgery and highlighted the inadequate figure of the surgeon as an evaluator of complications. It seems that spinal surgeons underestimate the complications impact on the patients and health system. As in a football game, the winning team usually maintains the best balance between the offense and defense units; in comparison, surgeons probably represent a really good offense unit (mission), but they lack in defense, where Chen’s reviewers demonstrated to be the better unit in that area (safety). The question to be addressed is what should be the first, mission or safety? We need an independent reviewer team (defense unit) to reduce complications and improve safety, and in doing so, we will probably improve clinical outcomes as well.
In this retrospective study, we observed that the overall incidence of complications in our spine surgery center during 3 years was 17.3%. We divided the complications into seven categories: hematoma, infection, cerebrospinal fluid (CSF) leakage or fistula, mechanical complications, neurological damages, systemic complications, and surgery-related death. This is probably the main weakness of the study: As the collection of complications started using a non-standardized system inserted in the hospital medical charts, any known classification system (as Glassman’s, Clavien–Dindo’s or SAVES systems) was used [25,26,27,28]; this probably caused an underestimation of the number of complications captured.
The most frequent complications observed in the current study were wound infections (5.5%), mechanical complications (4.4%), and neurological damages (3.2%). In our study population, almost 95% of the patients were affected by oncologic and degenerative diseases; we observed a trend to a higher wound infection complications (7.4%) in oncologic patients, while a trend to a higher rate of mechanical complications (5.8%) was observed in patients with degenerative diseases, even in the absence of statistical difference (p = 0.12).
This study found no correlation between diagnosis and overall complications’ incidence (p = 0.48). This was different from other large-scale studies which report a higher incidence of complications in patients undergoing surgery for oncological pathologies [8, 9, 32, 33]. This could be mainly due to the long experience of the authors in tumor spinal surgery [34,35,36].
This study found a rate of early complications (arising within 1 month after surgery) of 43.3%, a rate of complications requiring surgical revision of 7.6%, and a rate of neurological sequelae causing permanent damage of 2.4%. These types of complications have a relevant impact on the health system and, especially, the last two categories on the patients’ quality of life and clinical outcomes.
Considering the high incidence of complications in spine surgery, during the last years several authors focused their attention on the risk factors related to the onset of complications and on predictive models of complications after spine surgery [12,13,14,15,16].
Moreover, several preventive measures have been studied and recently described in order to reduce complications in spine surgery, concerning intraoperative neuromonitoring, blood loss reduction, and infections and thrombosis prophylaxis [19,20,21,22,23]. Sethi et al. [24] reported their experience concerning the application of Lean methodology in orthopedic surgery and specifically in spine surgery. Lean methodology was developed in the manufacturing industry to increase output and decrease costs, and then, it was implemented in many areas of health care. The authors described a step-by-step process designed specifically to optimize and standardize preoperative, intraoperative, and postoperative care for patients undergoing complex spine surgery, and they reported a significant reduction in overall complication rate [24].
In 2009, Haynes et al. [18] developed a 19-item Surgical Safety Checklist (SSC) to improve intraoperative outcomes and minimize preventable complications, thus making the culture of the operating theater safer, more communicative, and more collaborative. This checklist derived from an implementation of the Surgical Safety Checklist elaborated by WHO in 2008.
Although several investigators have challenged the efficacy of the SSC, it has shown repeated success in reducing preventable postoperative complications, length of hospital stay, and overall mortality [18, 37,38,39]. In addition, multiple investigators have concluded that the implementation of the SSC in multiple institutions has improved communication, efficiency, and attention to routine details in the operating room.
In the present study, we investigated, as preventive measure to reduce complications in spinal surgery, the introduction of the WHO Safety Surgical Checklist. Results showed a reduction in the overall incidence of complications following the introduction of the WHO Safety Surgical Checklist: In 2010, without the use of the checklist, the incidence of complications was 24.2%, while in 2011 and 2012, following the checklist introduction, the incidence of complications was 16.7% and 11.7%, respectively (mean 14.2%) (p < 0.0005). From our knowledge, this is the first report about the application of the WHO Surgical Safety Checklist in spinal surgery.
The only other reason that may have cooperated in the reduction in postoperative infections rate was the introduction in our institute of a new internal guideline for the prevention of infections in spine surgery (dated 07/20/2010) which has slightly changed the type of antibiotic drugs used for prophylaxis (one modified drug among five drugs used). However, the trend to the reduction in overall complications can be attributed to the introduction of the WHO checklist. In our experience, most of the alerts highlighted by the WHO checklist were really useful to do the right action in the right moment to avoid complication; in particular the questions contained in the Time Out section: Surgeon reviews: “What are the critical or unexpected steps, operative duration, anticipated blood loss?” and Anaesthesia team reviews: “Are there any patient-specific concerns?”improved the surgical team interactions and led to changes in surgical and anesthesiological procedures during the intervention that really allowed to avoid complications. The other question contained in Time Out section “Nursing team reviews: has sterility (including indicator results) been confirmed? Are there equipment issues or any concerns?” allowed to discover, before the beginning of the intervention, contaminated implants or surgical devices, skipped from the previous control, and led to avoidance of postoperative infections and other mechanical complications.
This study presents some limitations. First, it is a retrospective study where a non-standardized system was used for capturing the complications; therefore, complications can be incorrectly estimated. Second, our department performed spinal surgery mainly for oncological and degenerative diseases. Infection and trauma surgery occupied only a small proportion. Hence, the current study population cannot represent the generally common spinal surgery population, and this could lead to a certain degree of bias in the results of the present study. In particular, the incidence of late complications (i.e., mechanical complications and wound infections) could be underestimated in the group of oncologic patients due to their shorter survival compared to the other groups of spine diseases. However, the baseline distribution of the preoperative diagnosis categories had about the same proportion over time, and late complications normally impact on the non-oncologic group of patients, who represent the 45.58% of the study population. Third, the two groups compared were non-homogeneous in terms of patients’ number; patients treated in 2010 without the use of the WHO checklist were only 285, while patients treated in 2011 and 2012 with the use of the WHO checklist were 632.
Despite the aforementioned limitations, the WHO Surgical Safety Checklist resulted to be effective in reducing complications in our center. We think that a system, based on the Surgical Safety Checklist, should be introduced also during the preoperative and postoperative phases, in order to highlight all the specific moments where complication risk factors arise also in these phases. The checklist should be adapted for the specific spinal surgery characteristics. Finally, the introduction and validation of this checklist, implemented for preoperative, intraoperative, and postoperative phases, should be followed by the identification of targeted actions to prevent complications and improve patients’ safety.
Correspondence to Giovanni Barbanti-Brodano.
The authors declare that they have no conflict of interest.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Below is the link to the electronic supplementary material.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.