Readmission Rates, Reasons, and Risk Factors in Elderly Patients Treated With Lumbar Fusion for Degenerative Pathology
Varun Puvanesarajah, MD; Ali Nourbakhsh, MD; Hamid Hassanzadeh, MD; Adam L. Shimer, MD; Francis H. Shen, MD; Anuj Singla, MD
Spine. 2016;41(24):1933-1938.
Abstract
Study Design. Retrospective database review.
Objective. To determine readmission rates after 1 to 2 level, primary, elective lumbar spinal fusion surgery for degenerative pathology and elucidate risk factors that predict increased risk of 30-day readmission
Summary of Background Data. Early postoperative readmissions after spine surgery represent a significant source of increased cost and morbidity. As the elderly population represents a demographic with a growing need for spine surgery, readmissions within this population are of significant interest.
Methods. Medicare data (2005–2012) from an insurance database was queried for patients who underwent primary 1 to 2 level posterolateral lumbar spine fusion surgeries for degenerative lumbar pathology. After applying specific exclusion criteria to select for elderly patients (65–84 yr) undergoing mostly elective procedures, 52,567 patients formed the final study population. Readmission rates for medical, surgical, and all reasons were calculated within 30 days, 90 days, and 1 year postoperatively. Risk factors for medical, surgical, and all 30-day readmissions were also determined.
Results. Within 30 days, 90 days, and 1 year, 1510 (2.9%), 2776 (5.3%), and 6574 (12.5%) patients were readmitted, respectively. At 30 days, surgical diagnoses constituted 50.1% of all readmissions. Wound infection was the reason for readmission in 25.8% of all readmissions within 30 days. Diagnoses of chronic pulmonary disease (OR 1.41 95% CI 1.22–1.63), obesity (OR 2.20 95% CI 1.90–2.54), and positive smoking history (OR 1.33 95% CI 1.15–1.54) were associated with increased risk of surgical readmission.
Conclusion. Elderly patients undergoing lumbar spine fusion experience 30-day, 90-day, and 1-year readmission rates of 2.9, 5.3, and 12.5% for both medical and surgical reasons. Surgical site infection and wound complications are the most common surgery-related reasons for readmission. Medical diagnoses are more predominant during later readmissions, highlighting the comorbidity burden present in elderly patients.
Level of Evidence: 4
Introduction
Early postoperative complications represent a significant source of increased cost and morbidity after surgical procedures. Costs are increased even further when such complications result in new in-patient readmission.[1] As such, there has been a recent focus by the Centers for Medicare and Medicaid Services to reduce readmissions by instituting a system, whereby hospitals with higher readmission rates during the 30-day period after certain core surgical procedures are penalized by not receiving full reimbursement.[2–4] From a health economics perspective, it is possibly too early to understand the full scope of how this has impacted medical practice, given that several years into this program, many hospitals still incur large penalties.[5] However, unplanned, postoperative readmissions represent significant morbidity after surgery and a better understanding of the reasons and risk factors for these events are necessary for both proper patient education and optimizing healthcare.
Healthcare optimization is particularly important when considering elderly patients undergoing spine surgery. Often burdened with comorbidities, elderly patients are increasingly seeking spine surgery for degenerative pathology of the lumbar spine, with lumbar fusion rates in elderly Medicare beneficiaries increasing from 0.3 per 1000 enrollees in 1992 to 1.1 per 1000 in 2003.[6] Unfortunately, this demographic sector of the population is poorly studied, with regard to readmission rates. After lumbar spine surgery in patients of all ages, however, rates of 30-day readmission after lumbar spine procedures are well documented, estimated to be around 4.6%.[7] Recent data pertaining to analogous numbers in elderly patients is lacking.
Given the rapidly increasing numbers of elderly patients treated with lumbar spine fusion surgery, more information is needed regarding readmission rates and reasons after this procedure. The primary aim of the present study is twofold: (A) to determine readmission rates after 1 to 2 level, primary, elective lumbar spinal fusion surgery for degenerative pathology, and (B) to elucidate risk factors that predict increased risk of readmission within 30 days.
Materials and Methods
A nationwide database with insurance data from the United States of America was utilized for this study. Aggregate data from all Medicare recipients from 2005 to 2012 was queried. Official waiver of institutional review board approval was obtained, due to the use of purely deidentified data that was previously acquired.
Database patients 65 to 84-year old who underwent posterior/posterolateral lumbar or lumbosacral spinal fusion surgery were identified using the ICD-9-CM procedure code 81.07. This cohort of patients was then further narrowed to only include patients treated with 1 to 2 level spinal fusion surgery (ICD-9-CM: 81.62) with a diagnosis of degenerative lumbar spine condition on the same day of surgery (Table 1). Exclusion criteria included presence of prior spine trauma or infection of the spine, prior malignant cancer diagnosis (ICD-9 CM: 140.xx-209.3x), revision surgery, 3 level or greater surgeries (ICD-9-CM: 81.63, 81.64), any other spine fusion surgery on the same day as the index procedure, or anterior lumbar spine fusion during the 3 months prior to the index procedure, to exclude staged procedures. The dataset was further narrowed by excluding all patients treated with total hip replacement (ICD-9 CM: 81.51), total knee replacement (ICD-9 CM: 81.54), total shoulder replacement (ICD-9 CM: 81.82, 81.88), any de novo spine fusion, or any patients with a readmission diagnosis code pertaining to health services for specific procedures and aftercare (ICD-9 CM: V50.xx-V59.xx) in the year after the index procedure. The latter exclusion criteria intended to ensure that readmissions for a planned procedure unrelated to the index procedure and pathology were excluded. After applying inclusion and exclusion criteria, a cohort of 52,567 patients formed the study population.
The population was then assessed for primary ICD-9 diagnosis codes associated with readmissions during the 30 days, 90 days, and 1 year after the index procedure. For later time points (i.e., 90 days and 1 year), data was specifically stratified to only reflect patients with readmissions during those time periods who did not have earlier readmissions. Specifically, reported data concerned new readmissions within 30 days, within 30 to 90 days, and within 90 days to 1 year. Output readmission codes were coarsely categorized as medical, surgical, or "other." Diagnosis codes that fell into the surgical category were directly attributable to lumbar spine pathology (degenerative pathology, lumbar fracture); surgical complications (i.e., dural tear, infection, wound complications); implant-related complications; or postoperative pain. Degenerative lumbar spine diagnosis codes were grouped with surgical readmissions as it was estimated that most of these were likely coded to indicate a complication or persistent symptomatology not alleviated by the procedure. The "other" category encompassed diagnosis codes that did not fall into either medical or surgical complication categories, including codes related to trauma and other orthopaedic diagnoses that were not related to the lumbar spine and could not be directly attributable to surgery. The mean hospital cost of a readmission that occurred during the first year after surgery was recorded, as judged by actual Medicare reimbursement, as opposed to hospital charges.
After categorization of ICD-9 primary diagnosis codes, specific risk factors for medical, surgical, and all readmissions within 30 days were assessed. Patient characteristics that were queried for this purpose included sex; age, stratified by an age of 75 at the time of the index procedure; obesity; smoking status; and various comorbid diagnoses that included peripheral vascular disease (PVD), chronic pulmonary conditions, diabetes mellitus and osteoporosis.[8] For this analysis, each patient was assessed for one of these diagnosis codes at any time during their full set of records, which could extend at most 8 years. This was to prevent data skew due to poor coding practices of ICD-9 codes pertaining to comorbidity diagnoses,[9] with the reasoning that any of the aforementioned characteristics would negatively impact patients' health in a chronic fashion that would likely be difficult to reverse assuming a significant change within the 8-year snapshot of patient records.
Statistical Analysis
Pearson x 2 analysis was used to assess for whether or not certain cohorts of patients with a given diagnosis or characteristic had a greater propensity for having a readmission within 30 days. For all analyses, significance was set at P <0.001.
Results
Of the 52,567 patients included in this study, 19,471 (37.0%) were male and 16,698 (31.7%) were 75 years of age or older at the time of the index procedure. Of note, positive smoking status, obesity, diabetes mellitus, and chronic pulmonary disease were observed in 36.2, 24.6, 36.2, and 35.7% of patients, respectfully. Characteristics of the study cohort are provided in Table 2.
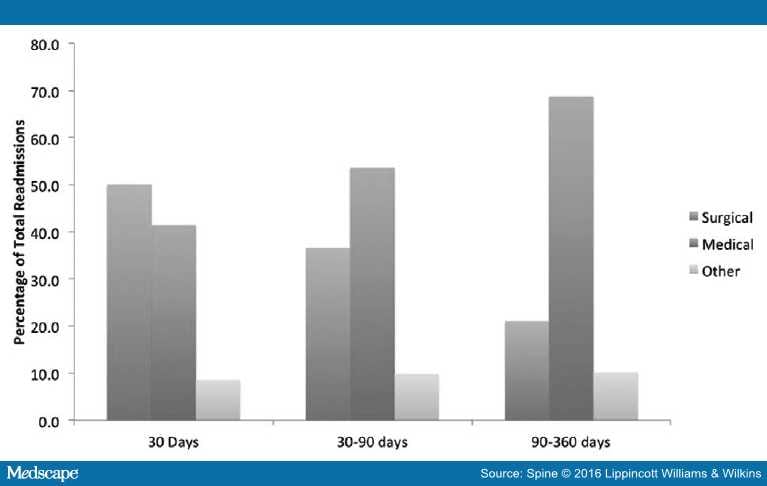
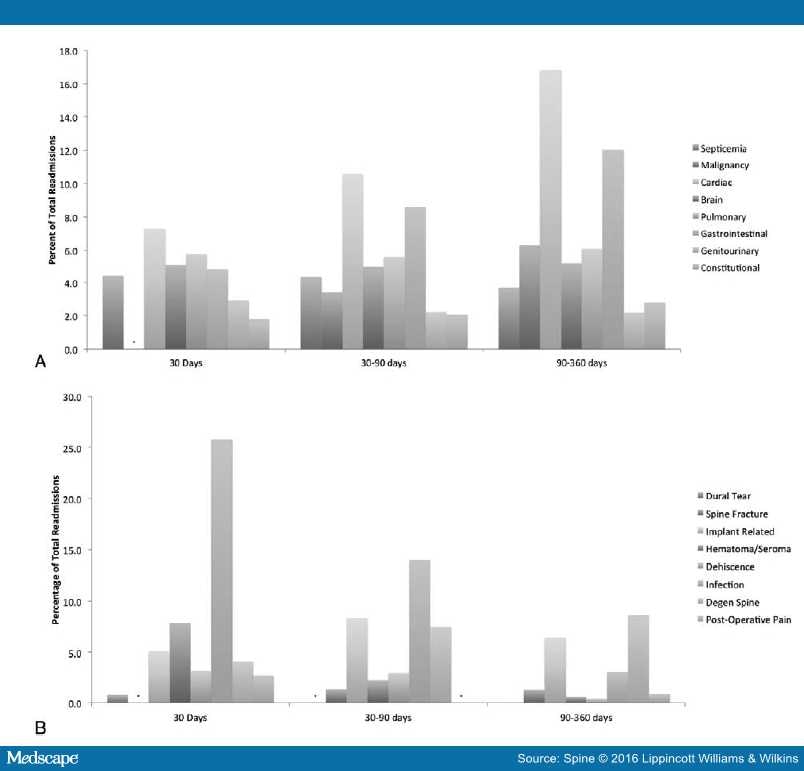
Within 30 days, 30 to 90 days, and 90 days to 1 year, 1510 (2.9%), 1266 (2.4%), and 3798 (7.2%) patients were readmitted, suggesting overall 30-day, 90-day, and 1-year readmission rates of 2.9%, 5.3%, and 12.5%, respectively. The full breakdown of primary diagnoses for readmissions within each time period is provided in Figures 1 and 2(A andB). At 30 days, surgical diagnoses constituted 50.1% of all readmissions. This decreased to 36.6% and 21.1% at 30 to 90 days and 90 days to 1 year, respectively. Paralleling this decrease was a progressive increase in the proportion of patients with medical readmissions (41.4%, 53.6%, and 68.8%, respectively). Surgical readmissions were most often due to surgical site infection during each period of follow-up. Infection was the reason for readmission in 25.8% of all readmissions within 30 days, though this number decreased to 14.0% by 30 to 90 days and 3.1% by 90 days to 1 year. Other common surgical reasons included implant-related complications, hematoma/seroma formation, or degenerative lumbar spine diagnoses. Medical readmissions were most commonly due to cardiac pathology, though gastrointestinal and nonspine central nervous system pathology were both notably frequent. The mean Medicare reimbursement associated with readmission within 1 year was $12,289 ± 13,346.
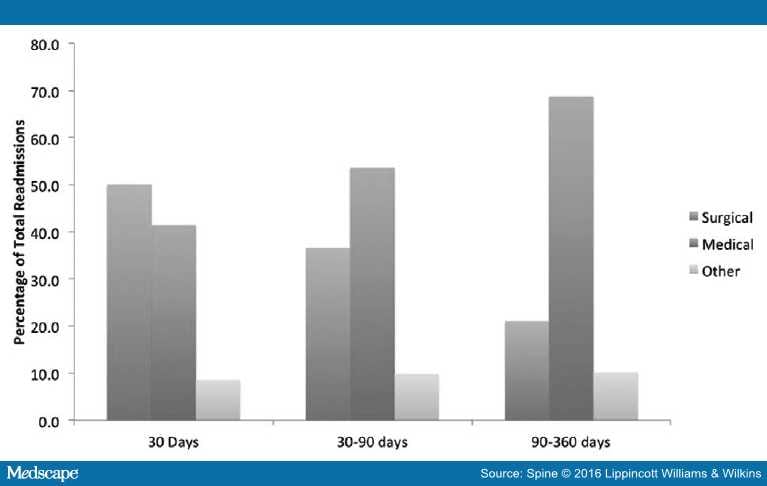
Figure 1.
Percentage of readmitted patients with medical and surgical primary diagnosis codes at 30 days, 90 days, and 1 year.
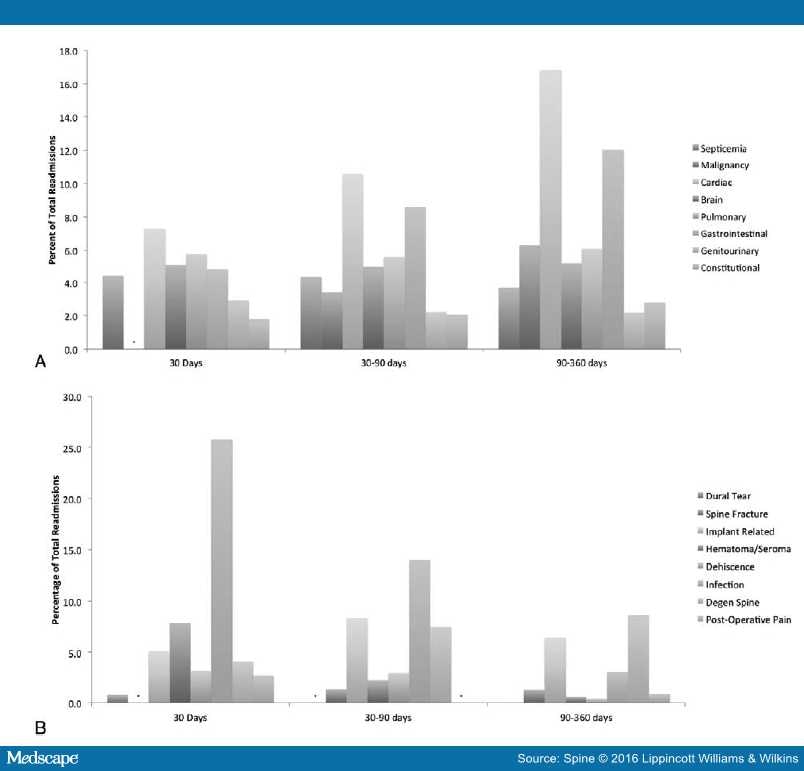
Figure 2.
Percentage of readmitted patients with specific medical (A) and surgical (B) diagnosis codes. * indicates percentages corresponding to raw output numbers less than 11.
Analysis of risk factors for medical, surgical, and all readmissions within 30 days are summarized in Table 3. Notably, diagnoses of chronic pulmonary disease (OR 1.41 95% CI 1.22–1.63), obesity (OR 2.20 95% CI 1.90–2.54), and positive smoking history (OR 1.33 95% CI 1.15–1.54) were associated with increased risk of surgical readmission. Of the assessed risk factors, only osteoporosis, sex, and surgery-day neurologic deficit diagnosis were not predictive of readmission due to any reason.
Discussion
Readmissions during the postoperative period can constitute a significant source of healthcare cost and morbidity in patients treated with spine procedures. As such, it is of utmost importance that spine surgeons understand the full scope of reasons for readmission after routine spine surgery in the elderly population, which represents a burgeoning sector of society with increased spine surgery needs. In the current study, we report 30-day, 90-day, and 1-year readmission rates of 2.9, 5.3, and 12.5% after primary elective 1 to 2 level lumbar spine fusion for degenerative pathology in an elderly population. New readmissions within 30 to 90 days and 90 days to 1 year were 2.4% and 7.2%, respectively. Infection was a common primary diagnosis for readmission and was listed as a reason for readmission in over 25% of patients readmitted within 30 days. Furthermore, at 30 days, chronic pulmonary disease, obesity, and smoking history were significant risk factors for surgical readmission, while, with the addition of peripheral vascular disease, diabetes, and older age, were also risk factors for readmissions for all reasons.
Many previous studies have investigated readmission rates after lumbar spine surgery. Using the American College of Surgeons National Surgical Quality Improvement Project database, Pugely et al estimated that 4.4% of patients had an unplanned readmission within 30 days after all lumbar surgeries for any indication. Subanalysis of only the population of patients treated with lumbar spine fusion surgery (4361 patients) yielded a 30-day readmission rate of 5.4%,[10] which is slightly higher than the 30-day readmission rate (2.9%) observed in the present study of a larger and relatively homogenous patient cohort. Other studies in patients treated with inpatient lumbar discectomies, lumbar decompressions, and laminectomy for lumbar spinal stenosis reported 30-day readmission rates of 6.7%,[11] 4.4%,[12] and 3.7%,[13] respectively. Given the increased age of our population, which has been associated with increased risk of readmission,[10,14] it is difficult to predict why our reported rate is lower than other studies, apart from possible explanation through the uniformity of our patient population through specific exclusion criteria that both intended to select for a more elective population and sought to exclude patients readmitted for other planned procedures during the follow-up period (4670 patients). However, our reported 90-day (5.3%) and 1-year (12.5%) readmission rates are higher than other studies, which have reported a 3.3% 90-day readmission rate after surgery for degenerative lumbar spine pathology[15] and 7.2% 1-year readmission rate after decompression surgery for lumbar spinal stenosis.[16] The latter study by Modhia et al[16] utilized a 5% sample of Medicare data, including patients of all ages, 87% of whom did not have concomitant fusion procedures. The increased 1-year readmission rate observed in our study could be due to an older population and increased procedural morbidity from fusion.
Although readmission rates varied slightly in comparison to other studies, reasons for readmission were similar. Within 30-days, Pugely et al[10] found that 38.6% of readmitted patients were diagnosed with a wound-related complication, a trend that has been observed in other series of spine surgery patients.[14,17,18] In comparison, 25.8% of the patients in our study were readmitted within 30 days with either a superficial or deep surgical site infection, 7.9% with either a hematoma or seroma, and 3.2% with dehiscence. However, beyond 30 days, medical reasons for readmission became much more prominent. In our study, 53.6% and 68.2% of readmitted patients had a medical primary diagnosis code within 30 to 90 days and 90 days to 1 year, perhaps reflecting the increased comorbidity burden observed in this patient population. Of medical reasons for later readmissions, both cardiac and gastrointestinal related diagnosis codes were more prominently observed. Interestingly, purportedly new diagnoses of malignancy, given prior exclusion of all patients with cancer, were observed in 3.8% of all patients readmitted within 1 year, highlighting both increased cancer incidence observed in the elderly population as well as incidental diagnosis while being admitted for other reasons.
Apart from delineating readmission rates and reasons for readmission, an additional aim of this study was to assess which preoperative factors resulted in increased risk of readmission. Advanced age[10,14]and chronic pulmonary disorders[10,18] were both found to be significant risk factors for readmission, a finding that has been echoed by other studies. Previous studies have also demonstrated that a higher American Society of Anesthesiologists score, a surrogate measure for comorbidity burden, is associated with an increased readmission rate.[10,12,13] This is similar to our finding that a number of medical comorbidities are associated with increased risk of readmission. However, our study is the first to determine specific risk factors for readmission for surgical reasons. Given that wound complications constitute a significant portion of surgical readmissions, the association of obesity (OR 2.2) and smoking history (OR 1.3) with surgical readmissions is plausible, since obesity[19–22] and smoking history[23,24]have both been correlated with infection and wound breakdown after spine surgery. Chronic pulmonary disease, another predictor of an increased risk of surgical readmission, has similarly been previously correlated with reoperation for wound complications.[25]
The present study has several strengths related to population size. By using a large, national, insurance database, we were able to select for a reasonably sized, uniform population of elderly patients to accurately determine expected readmission rates after elective lumbar 1 to 2 level spine surgery. However, our study has certain limitations that must be considered. ICD-9 coding error, in terms of comorbid diagnoses, procedures, and outcomes,[26] can hinder analysis and skew results. Second, the database utilized for this study involves use of purely aggregate data to allow for efficient data querying, which prevents multivariate analysis and other sophisticated statistical methods. Last, we may have not been able to fully exclude all planned procedures during the 1-year postoperative period. Although hip, knee, and shoulder replacements and additional spine fusions likely contribute the majority of elective surgeries that require in-patient hospitalization, other surgeries, including elective cholecystectomy, were not screened due to lack of clarity from ICD-9 coding concerning their elective nature. This limitation is likely more significant when considering 90-day and 1-year readmissions. Though these limitations are significant, we were able to successfully analyze readmissions in a large cohort of elderly lumbar spine fusion patients.
Conclusion
Elderly patients treated with primary elective 1 to 2 level lumbar spine fusion for degenerative pathology experience 30-day, 90-day, and 1-year readmission rates of 2.9, 5.3, and 12.5% after surgery. Wound complications represent over a quarter of all readmissions within 30 days. Obesity, smoking history, and chronic pulmonary disease are significant risk factors for surgical readmission within 30 days.