The diversity among the current international practice patterns and the discrepancy between the eminence-based medicine and the evidence-based medicine in the treatment of lumbar disk herniation is presented. Minimally invasive techniques were expected to give the lowest postoperative low back pain, however, also to give the highest risk of recurrent disk herniation.
Study Design. A questionnaire survey.
Objective. To evaluate the current practice patterns of surgeons regarding both the surgical and nonsurgical management of lumbar disk herniation (LDH) worldwide and to compare this with the current literature.
Summary of Background Data. Sciatica is a common diagnosis in the general population. Sciatica is most frequently caused by LDH. Multiple surgical techniques and treatment modalities are available to treat LDH, albeit some with small effect sizes or without compelling evidence.
Methods. A survey including questions on the application of physical examination, expectations regarding different surgical and nonsurgical techniques, factors influencing the outcome of surgery were distributed among members of AOSpine International and the European Association of Neurosurgical Societies.
Results. Eight hundred and seventeen surgeons from 89 countries completed the questionnaire. These surgeons perform a total of 62.477 discectomies yearly. Pain medication and steroid injections were expected to be the most effective nonsurgical treatments. The severity of pain and/or disability and failure of conservative therapy were the most important indications for surgery. A period of 1 to 2 months of radiculopathy was regarded as a minimum for indicating surgery. Unilateral transflaval discectomy was the procedure of choice among the majority and was expected to be the most effective technique with the lowest complication risk. Surgeons performing more lumbar discectomies, with more clinical experience and those located in Asia, were more likely to offer minimally invasive surgical techniques.
Conclusion. This study shows that current international practice patterns for LDH surgery are diverse. There seems to be a discrepancy between preferred surgical techniques and the attitudes of surgeons worldwide and the evidence. Further research should focus on developing international guidelines to reduce practice variety and offer patients the optimal treatment for LDH.
Level of Evidence N/A
Sciatica is defined as radiating pain from the buttock downwards to the leg.[1–3] Other symptoms may include low back pain, paresthesia, muscle weakness, or reduction of reflexes. Sciatica is most frequently caused by lumbar disk herniation (LDH), followed by spondylolisthesis, synovial cyst, and piriformis syndrome. Because of differences in study populations, acquisition of data, and definitions of sciatica, the reported prevalence of sciatica varies in the literature from 1.6% to 43%.[4]
The natural course of symptomatic LDH is favorable due to resolution of leg pain in the majority of the cases without the necessity of surgery.[5] About 33% of the patients visiting a general practitioner will recover within 2 weeks, which will increase to 75% after 3 months.[6] Nonsurgical therapy may include various strategies, including steroid injections, physical therapy, bed rest, manipulation, or medication while strong evidence is frequently lacking due to small effect sizes or high risks of bias amongst others. Surgery is usually considered when leg pain persists or progressive neurologic deficits develop.[7] According to Dutch guidelines, surgery is indicated when at least 6 to 8 weeks of conservative treatment has failed. There is no international consensus on the treatment strategy of symptomatic LDH and comparison of international back surgery rates may be difficult due to variations in health care systems.[8]
A randomized controlled trial comparing early surgery versus prolonged conservative management in patients with symptomatic LDH showed no differences between the two groups in functional disability or leg pain on both the short and long-term.[9–11] Patients who underwent early surgery reported faster pain relief and recovery. There were no differences in costs between surgery and conservative care. The cost-utility ratio was [Euro sign]41,000 per QALY gained and the probability that surgery is cost-effective compared with conservative treatment was 76% at [Euro sign]40,000 per QALY and 87% at [Euro sign]80,000 per QALY.[12]
Oppenheim and Krause[13] were the first to report on the surgical treatment of a ruptured intervertebral disk in 1909. Due to innovation and development, surgical approaches have evolved and nowadays different surgical techniques, such as micro-endoscopic discectomy (MED), often also referred to as micro-tubular discectomy (MTD), and percutaneous endoscopic lumbar discectomy (PELD), are being practiced worldwide.[14–19] The rationale behind most of these novel surgical techniques is to reduce the invasiveness, hospitalization, and rehabilitation. Despite these alternative surgical approaches, conventional open microdiscectomy still is regarded as the gold standard for surgical treatment of LDH.[20–23]
In 2008, the results of a survey on the treatment of LDH in the Netherlands were published.[24] That survey assessed the surgical management as of 2004 and differences in clinical practice and attitudes towards different surgical techniques were observed. These could be explained by the lack of high-quality evidence and consensus. Meanwhile, multiple randomized controlled trials have been published providing level I evidence on the efficacy of certain surgical techniques and treatment modalities albeit some without compelling evidence and small effect sizes.[11,19,25–27] Therefore, one might expect that the gap between eminence-based medicine and evidence-based medicine in the current treatment of LDH will be shortened. By the means of this study, the authors attempt evaluate the current practice patterns and to compare this with the current available literature.
Methods
The survey conducted by Arts et al[24] was modified by adding questions regarding physical examination, factors influencing the outcome of surgery, and the use of patient reported outcome measures (PROMs) (see online supplementary material, http://links.lww.com/BRS/B283). Questions regarding the operative techniques were extended by including full-endoscopic techniques, as these techniques are gaining popularity among both patients and surgeons.[18] The final survey consisted of 20 questions regarding (1) demographic characteristics, (2) presurgical management and expectations of nonsurgical treatments, (3) surgical techniques and expectations of those techniques, (4) postoperative management, and (5) the use of PROMs. Questions regarding physical examination, standard surgical procedures used, and advise on timing of resuming daily activities were answered by using a 3-point Likert scale. Expectations regarding both surgical and nonsurgical treatments, and factors influencing indication for surgery were rated on a 5-point Likert scale.[28,29] To test the face validity and comprehension, a pilot survey among a subset of neurosurgeons and orthopedic surgeons was performed before starting the final survey.
Between October 2015 and December 2015, an invitation to participate in the online survey (hosted on SurveyMonkey, Palo Alto, CA) was sent to all members of the European Association of Neurosurgical Societies (EANS) and of AOSpine International. EANS is a professional organization encompassing 1500 members, mostly European neurosurgeons. AOSpine is a worldwide community of 6179 members, mostly spine surgeons. To improve the response rate, a reminder was sent to members of both organizations. Residents and respondents who did not perform surgery for LDH were excluded for analysis.
Descriptive statistics were used to define characteristics of the surgeons who responded and their expectations of different treatment modalities. All percentages are based on valid responses. For analyzing purposes of the answers on 5-point Likert scales such as "most and very," "less and least," "highest and high," "low and lowest" were trichotomized. Differences in continuous variables were analyzed using a t test. Three multivariate logistic regressions were employed to analyze the association between surgeon's demographics and characteristics and whether they offer minimally invasive surgery (i.e., MTD, PELD, or both). For the regression analyses no missing data were accepted. Descriptive statistics were analyzed using SPSS statistics 21.0 (SPSS Inc., Chicago, IL). Logistic regression analyses were performed using STATA version 12 (StataCorp LLC Texas, USA). Statistical significance was set at 0.05.
Results
A total of 817 surgeons completed the survey, resulting in a response rate of 10.6%. The majority of the surgeons (96.5%) were male. Surgeons were employed in 89 countries with the majority being active in Europe (Figure 1). 50.6% of the respondents were trained in neurosurgery and 49.4% in orthopedic surgery. The surgeons had a mean of 14.4 (±9.2) years of clinical practice (Table 1). The cumulative amount of lumbar disk surgeries performed were 62.477 per year, with an average of 76 disk surgeries performed annually per surgeon. Neurosurgeons performed a higher amount of procedures annually, compared with orthopedic surgeons (91 vs. 62, P < 0.001).
All surgeons, except one, performed one or more diagnostic tests during physical examination when LDH is suspected. The straight leg raising test and testing for muscle weakness were most frequently performed by 92.9% and 94.0% of the responders, respectively. The crossed leg raising test was the least performed technique with 36.1% stating that they either "sometimes" or "never" assessed it.
Figure 2 provides an overview of the expected effectiveness of different conservative treatment modalities. Pain medication was regarded to be the most effective treatment. The effectiveness of steroid injections, exercise therapy, and counseling (by general practitioner, neurologist, or neurosurgeon) were expected to be "highest" or "high" by many responders, ranging from 44.7% to 55.9%. Complementary and alternative therapy, such as acupuncture, was expected to be the least effective by almost 60% of the responders.
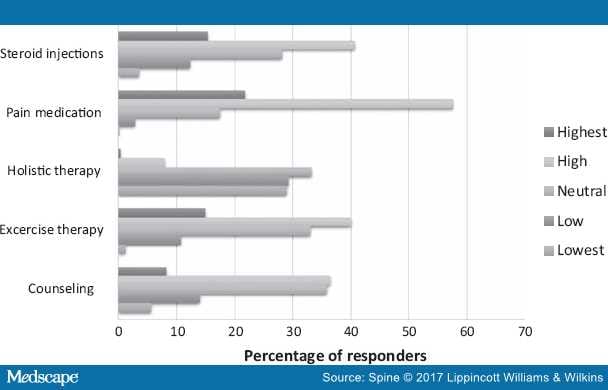 Figure 2.
Figure 2.
Perceived effectiveness of nonsurgical treatment modalities.
When indicating surgery, 46.1% of the surgeons regarded a period of 4 to 8 weeks of conservative treatment as the minimum. One-third regarded leg pain lasting for 8 to 12 weeks (23.0%), and more than 12 weeks (11.3%) as a minimum time period before deciding to perform surgery, while 19.5% of the surgeons who performed surgery within 4 weeks. Of these surgeons, more than one-fifth (N = 36), even reported to indicate surgery within 2 weeks.
Severity of pain and/or disability (55.3%) was considered to be the most import indication for surgery (Figure 3). Other important indications were failure of conservative treatment (50.6%), classic radiculopathy with neurological deficit (43.0%), and the duration of complaints (36.2%). The extent of the LDH and patient's preferences were less important indications.
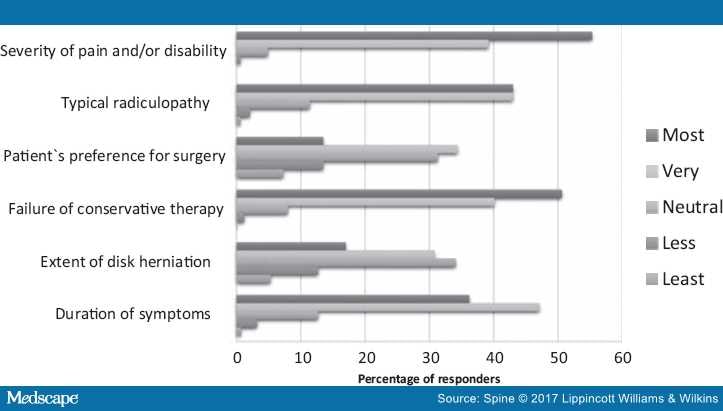
Figure 3.
Expected importance of clinical aspects of lumbar disk herniation to indicate surgery.
More than 80% of the surgeons reported to "usually" perform unilateral transflaval discectomy. Other frequently performed procedures were the MTD and bilateral muscle retraction with unilateral discectomy by 14.2% and 10.9%, respectively. Percutaneous laser disk decompression (PLDD) and PELD were performed the least, with 93.3% and 80.7% of the surgeons claiming to "never" perform these techniques (Figure 4). Multivariate logistic regression analysis revealed that surgeons performing a higher volume of discectomies annually, surgeons based in Asia and surgeons with more years in clinical practice were significantly more likely to offer minimally invasive surgery (P < 0.05, see Table 2). Furthermore, orthopedic surgeons were more likely to offer PELD (P < 0.001) as compared with neurosurgeons. Regarding the extent of disk removal during discectomy, 6.1% and 1.7% of the surgeons reported to remove the disk subtotally bilateral and completely bilateral, respectively. Unilateral limited disk removal and unilateral extensive disk removal was performed by 28.3% and 30.5% of the surgeons, respectively. The remaining 33.4% of the surgeons stated that they only removed the sequester in case of sequestration.
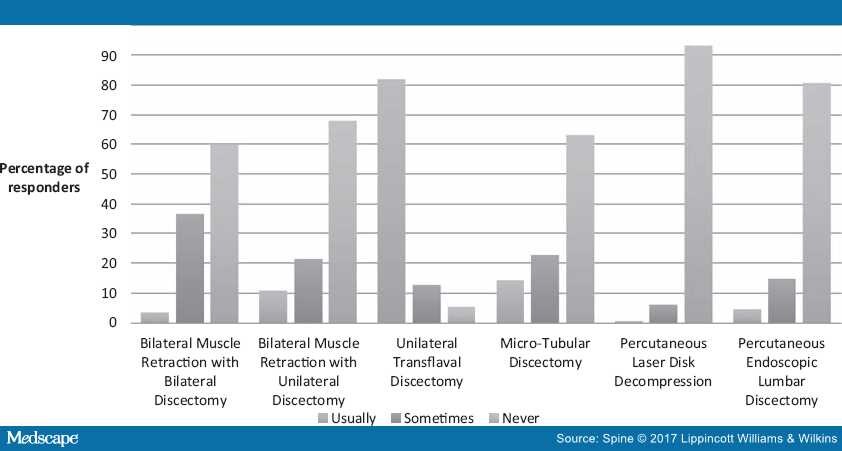 Figure 4.
Figure 4.
The performed operative techniques among the respondents.
Regarding the expectations of the different surgical techniques, unilateral transflaval discectomy was expected to have the highest effectiveness by 92.3% of the surgeons (Table 3) followed by MTD. More than half of the respondents estimated that PLDD would have the lowest effectiveness, followed by bilateral muscle retraction with unilateral discectomy. Regarding postoperative low back pain of the different techniques, PELD was expected to result in the lowest low back pain, followed by PLDD and MTD.
Concerning the risk of complications, more than two-third of the responders expected the unilateral transflaval approach to have the lowest risk. Surgical techniques expected to have the highest risk for complications were bilateral muscle retraction with either bilateral (38.6%) or unilateral (30.8%) discectomy. More than half expected that the risk of recurrent LDH would be the highest after PLDD. Other techniques with a high expected recurrent LDH were PELD (more than one-third of the surgeons) and MTD (more than a quarter of the surgeons). The lowest risk of recurrent LDH was expected after bilateral muscle retraction, with or without bilateral discectomy, and unilateral transflaval discectomy, with percentages ranging from 46.4% to 52.3%.
More than half of the surgeons reported to advise their patients to mobilize the same day of the surgery. One-third of these responders advised mobilization directly after returning to the ward, while the other two-third after a few hours (Table 4).
Directly after discharge, resumption of work and daily activities were never recommended by the majority of the surgeons, while almost 30% of the surgeons either sometimes or usually recommended resumption of work and daily activities directly after discharge. The majority recommended return-to-work and daily activities 4 or 6 weeks after surgery.
Figure 5 shows the expectations that surgeons have of different lifestyle factors that may mostly influence the outcome of surgery. A positive attitude and stress management, an exercise program, and a healthy weight with a lean body mass index, were expected to be the most important factors, with percentages ranging from 83.9% to 86.3%.
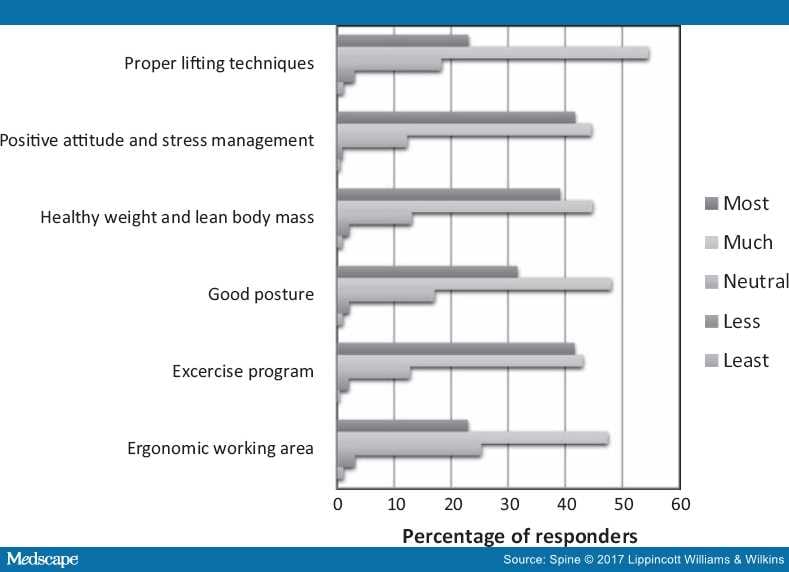 Figure 5.
Figure 5.
Factors influencing a good outcome after surgery.
Almost one-third of the surgeons reported not to register any PROMs. Visual analogue scores (VAS) for pain[30] were the most frequently used PROMs worldwide with 59.1% of the responders stating that their clinic keeps track of the VAS. The Oswestry Disability Index was used by 51.7% of the surgeons worldwide.[31,32] Documentation of the Functional Rating Index,[33] COMI-Back,[34,35] Roland-Morris Disability Questionnaire,[36,37] and Quebec Back-Pain Disability Scale[38] ranged from 2.7% to 9.2%. Other mentioned PROMs were EuroQol-5 dimensions questionnaire,[39] Short Form 12 and 36 surveys,[40–42] and the Japanese Orthopedic Association Back-Pain Evaluation Questionnaire.[43]
Discussion
The results of this survey provide an overview of the preferred surgical techniques and the attitudes of surgeons worldwide regarding both the surgical and nonsurgical management of LDH. Surgery for a symptomatic LDH is a frequently performed procedure among both neurosurgeons and orthopedic surgeons, with a wide variation in the number of discectomies performed per surgeon per year. More than 80% of the responders reported to "usually" perform unilateral transflaval discectomy. After the transflaval technique, MTD and bilateral muscle retraction with unilateral discectomy were the most performed techniques. More than 80% reported to "never" use PELD and more than 90% to "never" use PLDD.
In 2004, Arts et al[24] conducted a survey among Dutch spine surgeons in order to obtain an overview of the surgical management of symptomatic lumbar disk herniation. Among the 86 surgeons surveyed, unilateral transflaval discectomy was the most frequently performed technique and was also expected to have the highest effectiveness and the lowest risk for complications, which is also observed in the current survey. Expectations of surgeons worldwide in 2015 about minimally invasive techniques as MTD and PLDD were similar to the expectations of Dutch surgeons in 2004. These techniques were expected to give the lowest postoperative low back pain, but at the same time these techniques were expected to give the highest risk for recurrent disk herniation and a higher complication risk, compared with the transflaval approach. Timing of discectomy remained highly variable among the respondents.
Pain medication was thought to be the conservative treatment with the highest effectiveness, followed by steroid injections, exercise therapy, and counseling. Acupuncture was expected to have the lowest effectiveness of all the conservative treatments. Lewis et al[44] recently conducted a systematic review and network meta-analyses on the comparative effectiveness of management strategies for sciatica. In this study, considering overall recovery as the outcome of interventions, surgery, epidural injections, non-opioid analgesia, manipulation, and acupuncture showed a significant improvement compared with inactive controls or conventional care. Surgery and epidural injections were significantly superior to exercise therapy, percutaneous discectomy, and traction. With pain as the outcome, epidural injections and biological agents showed significantly superior results when compared with inactive control. Biological agents were the most likely to be the best treatment for pain relief, as compared with opioid and non-opioid medication, bed rest, and radiofrequency treatment. Overall, the authors concluded that the effectiveness of bed rest, opioid pain medication, exercise therapy, counseling as a therapy alone, traction, and percutaneous discectomy are not supported by their findings. Interestingly, exercise therapy and counseling were expected to have a "high" or "highest" effectiveness on sciatica, while pain medication was expected to be the highest effectiveness by the most respondents.
An adequate indication for surgery and the timing of discectomy have remained subject of debate throughout the years. The severity of pain and disability in daily functioning were the most important indications for surgery. The results of the Sciatica-trial showed that although patients who were randomized to early surgery recovered faster, functional outcomes at 1- and 2-years of follow-up were similar.[10,11,45] Remarkable was that of the 142 patients who were assigned to prolonged conservative treatment after an average of 9.5 weeks of sciatica, 55 (31%) of the patients eventually underwent surgery after a mean of 18.7 weeks while the remaining 87 (61%) patients didn't need surgery at all after 1 year of follow-up. These data emphasize the self-resolving character of sciatica in a substantial proportion of patients and warrants not offering surgery too early after the onset of radicular pain. Yet almost a fifth of the responders reported to regard a period of 4 weeks of radicular pain as a minimum for offering surgery.
During the past decade, more research has been conducted on the cost-effectiveness of MTD and PLDD. These two surgical techniques, along PELD, are usually dubbed as minimally invasive techniques, a name which already raises expectations as less tissue damage. Consequently, MTD, PELD, and PLDD were expected to give the lowest postoperative back pain and the speediest recovery. Interestingly enough, two robust randomized controlled trials comparing MTD and respectively PLDD with open microdiscectomy could not confirm these expectations. There was no significant difference in back pain of the patients who underwent PLDD compared with the control group, but the PLDD group had a significantly higher rate of reoperations.[25] Patients who underwent tubular discectomy reported even more back pain after 1-year of follow-up compared with patients who underwent conventional discectomy.[19] Furthermore, recovery of sciatica was similar in patients who underwent tubular discectomy compared with conventional discectomy. Despite the disappointing results of minimally invasive techniques, MTD and PLDD are still being performed "usually" or "sometimes" by 36.8% and 6.7% of the responders, respectively.
PELD was expected to give the lowest postoperative back pain. However, around 40% of the responders had a neutral expectation regarding the effectiveness, complication risk, and risk of recurrent disk herniation. There seems to be lack of a clear consensus on the advantages and disadvantages of this technique. A recently conducted meta-analysis concluded that patients who underwent endoscopic discectomy had a shorter hospitalization and less blood loss during surgery, while patients reported a significantly higher satisfaction rate compared with patients who underwent conventional open microdiscectomy. No significant differences were found in the complication rate, duration of surgery, and the rate of recurrent disk herniation. The authors concluded, however, that more high-quality randomized controlled trials with a sufficient sample size are necessary.[46] Coincidentally, a large randomized controlled trial assessing the cost-effectiveness of transforaminal PELD is currently being conducted.[47]
Some potential limitations of this study have to be acknowledged. As this study is a retrospective survey using non-validated questions, there will always be the risk of reporting and recall bias. Another limitation may be the interpretation of the Likert-scales, as they can be scored as relative of each other or as a stand-alone item. The impact of these disadvantages is limited, as it was our aim to evaluate the attitudes of surgeons worldwide. Both a strength and a limitation are the amount of responses received for this survey. A total of 817 surgeons from 89 countries completed the survey, which supports the generalizability of the results. However, it is inevitable that sampling bias has occurred as participating surgeons were all members of two professional organizations (e.g. EANS, AOSpine). Furthermore, orthopedic surgeons were from all continents and spine-dedicated. In contrast to this, the neurosurgeons were mostly from Europe and to a lesser extent spine dedicated. Because the survey was distributed to two organizations, the EANS and AOSpine International, the calculated response rate should be even higher because some surgeons are members of both organizations. Additionally, not all members were eligible to fill in the survey because we only included responses of surgeons who actually perform surgery for LDH. Furthermore, the response rate can be considered high, even when we compared our response rate with other surveys among spine surgeons or AOSpine members.[48–51]
Conclusion
This study presents the diversity among the current international practice patterns and the discrepancy between the eminence-based medicine and the evidence-based medicine in the treatment of LDH. Further research should focus on developing international guidelines to reduce practice variety and offer patients the optimal treatment for LDH.
References
Acknowledgments
The authors would like to acknowledge the funding provided by AOSpine and Mapchart.net for creating Figure 1. Furthermore, we want to thank the EANS and AOSpine International for distributing the survey.
The manuscript submitted does not contain information about medical device(s)/drug(s).
AO Spine International funds were received in support of this work.
Relevant financial activities outside the submitted work: consultancy, grants, royalties, travel/accommodations/meeting expenses.
Spine. 2017;42(23):1826-1834. © 2017 Lippincott Williams & Wilkins
Surgery Doesn't Trump Rehabilitation in Patients With Degenerative Disk DiseaseJournal Article
Management of Lumbar Conditions in the Elite AthleteJournal Article
Current Concepts in the Management of SpondylolisthesisJournal Article
 Sex Life and Impact of Operative Intervention on Sex Life-Related Pain in Degenerative Spinal ConditionsJournal Article
Sex Life and Impact of Operative Intervention on Sex Life-Related Pain in Degenerative Spinal ConditionsJournal Article
| Number of Respondents (%) | |
|---|---|
| Male | 773 (96.5) |
| Continent | |
| Africa | 33 (4.0) |
| Neurosurgeon | 12 (1.4) |
| Orthopedic surgeon | 21 (2.6) |
| Asia and Oceania | 195 (23.9) |
| Neurosurgeon | 62 (7.6) |
| Orthopedic surgeon | 133 (16.3) |
| Europe | 362 (44.3) |
| Neurosurgeon | 240 (29.4) |
| Orthopedic surgeon | 122 (14.9) |
| North America | 67 (8.2) |
| Neurosurgeon | 25 (3.1) |
| Orthopedic surgeon | 42 (5.1) |
| South America | 160 (19.6) |
| Neurosurgeon | 74 (9.1) |
| Orthopedic surgeon | 86 (10.5) |
| Lumbar disk surgeries performed annually | |
| 0–25 | 214 (26.2) |
| 26–50 | 328 (40.1) |
| 51–100 | 99 (12.1) |
| 101–200 | 137 (16.8) |
| More than 200 | 39 (4.8) |
| MTD | PELD | Minimally Invasive Surgery | ||||
|---|---|---|---|---|---|---|
| Variable | Odds Ratio (OR) | 95% CI of OR | Odds Ratio (OR) | 95% CI of OR | Odds Ratio (OR) | 95% CI of OR |
| Performed cases per year | ||||||
| 50–100 (ref. 0–50) | 1.21 | (0.81–1.80) | 2.12* | (1.28–3.52) | 1.29 | (0.87–1.90) |
| >100 (ref. 0–50) | 1.99*** | (1.34–2.93) | 4.55*** | (2.78–7.45) | 2.80*** | (1.89–4.14) |
| Surgical specialty | ||||||
| Orthopedics (ref. neurosurgery) | 1.06 | (0.76–1.47) | 2.19*** | (1.41–3.38) | 1.33 | (0.96–1.83) |
| Years of clinical experience | ||||||
| 10–20 (ref. 0–10) | 1.66** | (1.15–2.39) | 1.40 | (0.88–2.23) | 1.85*** | (1.29–2.64) |
| >20 (ref. 0–10) | 1.44 | (0.97–2.13) | 1.16 | (0.70–1.93) | 1.48* | (1.01–2.17) |
| Continent of practice | ||||||
| Africa (ref. Asia) | 0.23** | (0.09–0.60) | 0.24* | (0.07–0.83) | 0.20*** | (0.08–0.50) |
| Europe (ref. Asia) | 0.35*** | (0.23–0.51) | 0.32*** | (0.19–0.54) | 0.32*** | (0.22–0.48) |
| North America (ref. Asia) | 0.52* | (0.29–0.96) | 0.39* | (0.16–0.93) | 0.47* | (0.26–0.86) |
| South America (ref. Asia) | 0.46*** | (0.29–0.72) | 1.08 | (0.64–1.82) | 0.55** | (0.35–0.85) |
| Constant | 0.57* | (0.36–0.88) | 0.10*** | (0.06–0.18) | 0.57* | (0.37–0.89) |
| N† | 810 | 810 | 810 | |||
| Chi-square | 56.79*** | 82.27*** | 85.81*** | |||
| Pseudo R-square | 0.0565 | 0.114 | 0.0806 | |||
Minimally invasive surgery compromises both MTD and PELD. 7 of the 817 questionnaires were excluded for the logistic regression analysis because one or more of the data on the variables were missing. *0.05. **0.01. ***0.001. LDH indicates lumbar disk herniation; MTD, micro-tubular discectomy; PELD, percutaneous endoscopic lumbar discectomy.
| Effectiveness | Postoperative Low Back Pain | Complication Risk | Risk of Recurrent Disk Herniation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Most | Neutral | Least | Most | Neutral | Least | Highest | Neutral | Lowest | Highest | Neutral | Lowest | |
| Bilat. muscle retraction, bilat. discectomy | 34.6 | 31.0 | 34.4 | 74.4 | 18.7 | 7.0 | 38.6 | 33.1 | 28.3 | 15.8 | 31.9 | 52.3 |
| Bilat. muscle retraction, unilat. discectomy | 38.2 | 26.7 | 35.2 | 69.6 | 21.3 | 9.1 | 30.8 | 37.3 | 31.9 | 12.3 | 41.2 | 46.4 |
| Unilat. transflaval discectomy | 92.3 | 5.8 | 1.9 | 14.1 | 34.6 | 51.3 | 3.9 | 28.2 | 67.8 | 6.9 | 41.3 | 51.8 |
| MTD | 58.3 | 29.7 | 12.0 | 9.5 | 28.1 | 62.4 | 14.2 | 36.6 | 49.1 | 26.8 | 44.5 | 28.8 |
| PELD | 35.0 | 40.2 | 24.8 | 6.2 | 29.9 | 63.9 | 22.3 | 38.2 | 39.4 | 37.0 | 43.1 | 19.9 |
| PLDD | 8.6 | 34.2 | 57.2 | 5.8 | 30.8 | 63.4 | 19.1 | 41.4 | 39.5 | 51.9 | 34.9 | 13.3 |
LDH indicates lumbar disk herniation; MTD, micro-tubular discectomy; PELD, percutaneous endoscopic lumbar discectomy; PLDD, percutaneous laser disk decompression.
| Mobilization Postoperatively | Percentage of Responders | ||
|---|---|---|---|
| Day 0, directly after returning to the ward | 18.0 | ||
| Day 0, after few hours | 36.2 | ||
| Day 1 | 40.6 | ||
| Day 2 | 3.8 | ||
| Day 3 or later | 1.5 | ||
| Resuming Work and/or Daily Activities | Usually | Sometimes | Never |
| Directly after discharge | 6.7 | 22.8 | 70.5 |
| After 2 weeks | 27.6 | 51.2 | 21.2 |
| After 4 weeks | 48.5 | 42.4 | 9.1 |
| After 6 weeks | 48.5 | 30.0 | 21.4 |