Nicolas S. Piuzzi, MD; Paul Manner, MD, FRCSC; Brett Levine, MD, MS
J Am Acad Orthop Surg. 2018;26(20):e437-e441.
Abstract and Introduction
Osteoarthritis (OA) is the most common form of joint disorder in the United States, and it is estimated that >27 million (>10%) Americans are affected.[1] Specifically, the burden of OA of the hip is increasing because of the aging population and obesity crisis; as a result, the need for total hip arthroplasty (THA) is expected to grow 174%, to 572,000 primary THAs per year by 2030 in the United States, and to a greater extent throughout the world.[2–4]
Multiple risk factors, including age, obesity, genetics, activity-related risk factors, and others, have been identified for hip OA.[5] THA is a recognized and proven intervention for symptomatic patients with advanced OA of the hip.[6] However, despite excellent functional outcomes reported with THA, careful patient selection is needed to achieve best possible outcomes, and treatments need to be appropriately adapted to each individual patient.[6,7]Ideally, treatment decisions should be based on the high-quality unbiased literature. Unfortunately, the assessment and subsequent application of the available literature to specific everyday scenarios are not always forthright.
In December 2017, the American Academy of Orthopaedic Surgeons published the Appropriate Use Criteria (AUC) for the Management of Osteoarthritis of the Hip[8] to improve patient care by providing an evidence-based approach, in conjunction with the clinical expertise of physicians, for the use of nonpharmacologic and pharmacologic interventions for symptomatic OA of the hip and surgical procedures. Initially, four assumptions were agreed upon before applying the AUC that were developed (Table 1). On acceptance of these stated assumptions, the AUC can be used to establish what treatments are appropriate, may be appropriate, or rarely appropriate in specific clinical situations, as highlighted in the cases described in the following sections.
A 39-year-old woman (body mass index [BMI], 30.6; height, 162 cm; weight, 80.4 kg) presents with right-sided groin pain that has been worsening over the past 2 years. The patient reports being very active in the past, participating in gymnastics, running, and Pilates routines but denies any specific trauma to the right hip. Currently, groin pain limits her to ambulating less than in the past, but she can still walk 1 to 2 miles consecutively. She reports having trouble getting in and out of the car and feels like she has to lift and/or drag the right leg into the car. Overall, her hip flexion remains relatively good at 120°, and she can abduct to 40°. At extremes of motion, she has pain, particularly with the combination of flexion, adduction, and internal rotation; however, her range of motion is almost the same as her contralateral side. She has tried a series of nutraceuticals, NSAIDs and over-the-counter analgesics, physical therapy, and activity modification. She would like to be able to participate in her children's activities more and is even becoming clinically depressed with her lack of activity and increasing weight. The patient is interested in surgical intervention to restore her quality of life and improve her overall health. On review of her history and radiographs (Figure 1), the treating physician feels that she has mild OA with what is likely femoral acetabular impingement and/or a labral tear.

Figure 1.
PA (A) and lateral (B) radiographs of a hip with mild osteoarthritis and femoral acetabular impingement.
Using the AUC Surgical Management of Osteoarthritis of the Hip, her physician considers the following management options (Figure 2): risk factor assessment and optimization (score = 8), activity modification (score = 9), assistive devices (score = 7), oral medications (score = 8), and physical therapy (score = 8). The physician notes that all the nonsurgical management approaches have already been attempted and intra-articular steroid injections received a maybe appropriate management recommendation for her specific patient indications (score = 6). Surgical management approaches, including arthrodesis and arthroplasty (scores = 1 and 2, respectively), are listed as rarely recommended, whereas hip preservation is scored as 7 and appropriate for the management of this patient's hip condition.

Figure 2.
Management options and appropriateness ratings. Numbers in the procedure recommendations are the median scores of the American Academy of Orthopaedic Surgeons Appropriate Use Criteria for the Management of Osteoarthritis of the Hip Voting Panel. The scores are rated on a scale of 1 to 9: 1 to 3 = rarely appropriate, 4 to 6 = may be appropriate, 7 to 9 = appropriate, and + = agreement among panel members (ie, two panelists or one panelists outside the three-point range containing the median).
On the basis of her previous treatment history, activity level, and radiographs, she is referred to a hip preservation specialist for the management of the hip. Ultimately, she underwent an arthroscopy with repair of the labrum and preservation of her native hip.
An 85-year-old woman (BMI, 34.2; height, 157 cm; weight, 84.3 kg) presents with activity limiting right hip pain over the past 6 years that is rapidly progressing. She feels that her medical conditions are compounding and expresses fear that her diminishing functional capacity will greatly impede her future quality of life. She is still active, volunteering at the hospital and taking care of her great-grandchildren. However, because of pain in her right groin, she is now not driving and having a hard time putting on shoes and socks. Pain is also keeping her up at night, and she is unable to walk more than a block at a time. She has been through an extensive course of NSAIDs, physical therapy, and corticosteroid injections and is even now walking with the assistance of a cane. On physical examination, she has a 20° flexion contracture of the hip and internal rotation to neutral. Her hip flexion is limited to 90°, and she can adduct to neutral. She is unable to cross her right leg over the left while sitting. Radiographic evaluation of the right hip includes AP and lateral views (Figure 3A) and reveals severe OA of the right hip. The patient states that she does not wish to continue receiving injections and taking medications to control her symptoms because she feels that they are no longer providing her adequate relief.
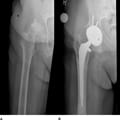
Figure 3.
PA (A) radiographs of a hip with severe osteoarthritis and (B) 5-year follow-up after total hip arthroplasty.
Using the AUC Surgical Management of Osteoarthritis of the Hip, her physician would consider only surgical interventions because the potential nonsurgical management approaches have been exhausted. According to the voting panel, arthroplasty is the only surgical intervention appropriate for this patient (score = 8), whereas hip preservation and arthrodesis are considered rarely appropriate (score = 1). All nonsurgical options are still considered appropriate with agreement but have already been tried without sustained relief of arthritic pain. These include risk factor assessment and optimization, activity modification, use of an assistive device, oral medications, intra-articular steroid injection, and physical therapy (Figure 4).

Figure 4.
Management options and appropriateness ratings. Numbers in the procedure recommendations are the median scores of the American Academy of Orthopaedic Surgeons Appropriate Use Criteria for the Management of Osteoarthritis of the Hip Voting Panel. The scores are rated on a scale of 1 to 9: 1 to 3 = rarely appropriate, 4 to 6 = may be appropriate, 7 to 9 = appropriate, and + = agreement among panel members (ie, two panelists or one panelists outside the three-point range containing the median).
On the basis of her history of management approaches and the appropriateness of surgical interventions, she underwent a hybrid THA (Figure 3, B) and recovered well, resuming her volunteer activities and childcare duties. She has felt that she has been able to restore her quality of life and better manage her medical comorbidities.
A 48-year old man with 3 months of left-sided groin pain presents for the first time to his practitioner's office. He has a history of type I diabetes mellitus with an hemoglobin A1c level of 10.6. Groin pain is present, but he is still able to ambulate a mile at a time without stopping and can still put on his shoes and socks, albeit with some difficulty. He is 177 cm tall and weighs 129 kg, with a BMI of ~41. He currently ambulates without assistive devices and has tried only an occasional dose of acetaminophen for pain. His pain is purely activity related, yet he maintains a near-symmetric pain-free range of motion of his hip. Overall, he has not restricted his activity level and is interested in what his current options are for his pain. Radiographic evaluation of the left hip includes AP, lateral, and PA pelvis views. Figure 5 shows hip AP radiographs which reveals mild OA of the hip.

Figure 5.
PA radiographs of a hip with mild osteoarthritis.
On the basis of the AUC Surgical Management of Osteoarthritis of the Hip, the patient is not a good candidate for surgical intervention with arthroplasty (score = 3), hip preservation (score = 2), and arthrodesis (score = 1) receiving rarely appropriate ratings. According to the voting panel, risk factor optimization, activity modification, oral medications, and physical therapy received an appropriate with agreement recommendation (score = 9). Intra-articular corticosteroid injections were rated as appropriate (score = 7), as well as assistive devices (score = 8) (Figure 6).

Figure 6.
Management options and appropriateness ratings. Numbers in the procedure recommendations are the median scores of the American Academy of Orthopaedic Surgeons Appropriate Use Criteria for the Management of Osteoarthritis of the Hip Voting Panel. The scores are rated on a scale of 1 to 9: 1 to 3 = rarely appropriate, 4 to 6 = may be appropriate, 7 to 9 = appropriate, and + = agreement among panel members (ie, two panelists or one panelists outside the three-point range containing the median).
In this case, the patient is not medically or physically optimized for surgery. Therefore, he was referred to the local wellness center and worked on weight loss to improve his BMI and gain better control of his diabetes. With targets of a BMI of <35 and an hemoglobin A1c level of <7.5, the patient enrolled in the program. With physical therapy and nutritional counseling, the patient lost 30 lbs and had improvement in his pain. He currently is taking an occasional dose of acetaminophen and ibuprofen and managing all activities of daily living without limitation. He would not like to proceed with any further intervention at this time and will follow-up if needed
OA of the hip is one of the most commonly seen diagnoses in orthopaedic practice. Patients presenting with OA of the hip have countless possible clinical scenarios, and it is improbable to establish uniform agreement among physicians as to the best way to provide nonsurgical and surgical care options for many of these patients. However, there is common belief that options for surgical and nonsurgical interventions must be individualized to each patient, with consideration for their severity of symptoms, age, functional status, and radiographic degree of involvement. To assist in the decision-making process, the American Academy of Orthopaedic Surgeons AUC Management of Osteoarthritis of the Hip tool considers expert opinion and the highest available quality evidence. The voting panel reviewed 270 scenarios to determine the ratings for each with crucial parameters mentioned earlier. The web-based application can be found at www.orthoguidelines.org/auc (http://www.orthoguidelines.org/go/auc/auc.cfm?auc_id=225000). This application can be used to help clinicians in developing a treatment plan for managing hip OA. Furthermore, it may be used to counsel patients about the appropriateness of the treatment provided in their particular clinical setting.