Hip Fractures: Current Review of Treatment and Management
Daniel C. Kim, MD, MS; Michael W. Honeycutt, MD; John T. Riehl, MD
Curr Orthop Pract. 2019;30(4):385-394.
Hip fractures are one of the most common major orthopaedic injuries in the United States, with an incidence that is growing with the aging population. These fractures vary significantly in anatomy, pathogenesis, and treatment. Orthopaedists must be able to carefully distinguish between femoral neck, intertrochanteric, and subtrochanteric femoral fractures because diagnosis is essential in guiding treatment. The extent of complex decision-making and management is often underappreciated in this diverse group of fractures. In this review, the relevant background, anatomy, and current treatment considerations essential to optimize management of these common and significant injuries are discussed.
The term "hip fracture" is a misnomer that is often used to refer to any fracture of the proximal femur extending from the distal extent of the femoral head to the proximal aspect of the femoral shaft. Acetabular fractures are not usually included in this terminology despite being a part of the hip joint and have separate diagnostic and treatment considerations. The fractures referred to in this anatomic region are classically divided into femoral neck (FN), intertrochanteric (IT), and subtrochanteric (ST) fractures, from proximal to distal, respectively. Proper diagnosis is an essential first step in understanding treatment options because they vary regionally along the "hip".
Hip fractures are one of the most common major orthopaedic injuries in the United States, with an incidence of 1.66 million worldwide in 1999, projected to rise above 6 million per year in 2050.[1] Management of hip fractures cost roughly $20 billion in 2010, and this diagnosis is consistently one of Medicare's top expenses.[2] In addition to the increase in hip fracture incidence over time, the diagnosis carries with it significant morbidity and mortality. Hip fractures carry a 20% to 30% 1-year mortality rate in elderly patients;[3] therefore carefully integrated care with a multidisciplinary approach is essential to improve outcomes.[4,5] It is important to keep in mind that the diagnosis of a low-energy hip fracture is more than just an orthopaedic diagnosis. It can be an indicator of systemic disease as well. In other words, people who are otherwise healthy do not often fall from ground level and break their hip. The goal of treatment in these fractures is early medical optimization and surgical stabilization to allow for quicker mobilization and recovery.
Because hip fractures are so common, the extent of complex decision making and management often is underappreciated in this diverse group of fractures. This review covers the relevant background, anatomy, and treatment considerations essential for an orthopaedic practitioner to optimize management of these common and significant injuries.
By the time the orthopaedic surgery team has been consulted, the diagnosis of a hip fracture often has already been determined. The clinical evaluation is similar among all hip fracture subtypes. For most displaced hip fractures, patients will have pain surrounding the entire hip region, and any movement of the affected limb generates significant pain. On visual examination, patients often have a resting lower extremity position of flexion, external rotation, abduction, and shortening. Patients with nondisplaced FN or IT fractures may complain only of mild pain in the groin and may be able to bear weight on the fractured extremity. On physical examination, nondisplaced fractures will not cause obvious clinical deformity, and patients will have moderate discomfort with hip range of motion.
As with all comprehensive orthopaedic trauma clinical evaluations, the patient should undergo a complete secondary survey to evaluate for other injuries in the setting of a distracting hip fracture. A thorough history is important for low-energy fracture mechanisms in determining treatment and disposition. This history should include a complete medical history, preinjury functional and ambulatory status, presence of prior hip pain, which could be indicative of a pathologic fracture and/or preexisting arthritis, and any loss of consciousness or history of syncope.[6]
The radiographic evaluation of hip fractures is critical to appropriate fracture management. It includes similar requirements for all hip fracture subtypes with a few notable differences. Recommended radiographs include an anteroposterior pelvis, cross-table lateral, and full-length femur radiographs of the affected side. Obtaining a frog-leg lateral view is less desirable because it can potentially cause displacement of a nondisplaced FN fracture.[6] Some surgeons prefer dedicated imaging of the uninjured hip to use as a preoperative template. The most valuable radiograph for specifically defining the FN or IT fracture pattern is a traction-internal rotation anteroposterior view of the hip, which accounts for normal FN anteversion and assists in preoperative planning.[7] A CT scan of the pelvis can be beneficial in characterizing the fracture pattern as well; however, CT scan is not the standard of care and is not routinely obtained in the radiographic workup of hip fractures. MRI or a bone scan can be used for evaluation of occult hip fractures. In the setting of a delayed presentation to the hospital, duplex ultrasound can be used to rule out deep venous thrombosis.
The initial treatment goal of hip fracture surgery is to allow early mobilization and weight bearing. It is not uncommon for post-injury functional status to decrease in elderly patients after hip fracture from the pre-injury state. Additionally, patients should be routinely screened for osteoporosis, and treatment should be provided as indicated.
FN fractures are proximal femoral fractures located in the region between the femoral head and the trochanters. Common risk factors for FN fractures include female gender, white race, tobacco and alcohol use, history of prior fracture, poor health, history of prior falls, and low estrogen levels.[8–10] FN fractures have a bimodal distribution in which the minority are caused by a high-energy mechanism in younger patients, and the majority are caused by low-energy falls in older patients.[11]
The femoral neck-shaft axis forms an angle of 120 to 135 degrees. The FN has an anteversion angle of approximately 10 to 15 degrees in reference to the posterior distal femoral condyles. The blood supply to the femoral neck is tenuous and is primarily served by the medial femoral circumflex artery with contribution also from the lateral femoral circumflex artery and a minor contribution from the artery of the ligamentum teres. The circumflex arteries form an extracapsular ring that gives off the ascending cervical branches. These branches provide retrograde blood flow to the femoral head.[12] One of the treatment challenges of FN fractures is that the FN has relatively inherent poor biological healing potential; most FN fractures are intracapsular and bathed in synovial fluid that inhibits angiogenesis, have a tenuous blood supply, and lack a periosteal layer. Thus healing is endosteal without the ability to form callus.[13]
Multiple classification systems have been developed for FN fractures, with the most commonly used being the Garden and Pauwels classifications (Figures 1 and 2). The Garden classification is the most frequently used in the literature and is divided into four subtypes based on fracture displacement.[14] Type I fractures are incomplete fractures (including valgus impacted fractures), type II are complete fractures that are nondisplaced, type III are complete and partially displaced, and type IV are complete and fully displaced. However, these subtypes can be difficult to distinguish, and a simplified Garden classification system has been developed that differentiates fractures as nondisplaced (subtypes I and II) versus displaced (subtypes III and IV). Close attention must be paid to the lateral view in femoral neck fractures because many times a fracture may appear valgus impacted (Garden I) on the anteroposterior view but will have posterior displacement on the lateral view (Figure 3). These fractures can have completely different treatments; therefore, diagnosis must be made with careful evaluation of all views. Other classification systems that are not mentioned in this manuscript have been described as well. Pauwels classification is subdivided into three types based on the angle of the fracture line from the horizontal. Type I is less than 30 degrees, type II is 30–50 degrees, and type III is greater than 50 degrees.[15,16] As the angle increases, shearing forces increase, and the risk of fracture displacement and varus collapse increase.[17] Fixed-angle devices for the treatment of higher-grade Pauwels fractures may be of benefit in resisting these forces and to prevent postoperative displacement. The AO/OTA classification is based on a comprehensive classification system that is primarily used for research purposes. The most important treatment and prognostic value of these classification systems is the presence of displaced or nondisplaced fracture fragments because this consideration is critical for determining vascularity and the risk of osteonecrosis. Additionally, FN fractures may be classified based on fracture location within the FN. The FN fracture may be divided into subcapital (directly adjacent to the femoral head), transcervical (mid-neck), and basicervical (low neck) fractures. The significance of location is that subcapital and transcervical fractures are intracapsular fractures, whereas basicervical FN fractures are extracapsular and therefore can be managed similarly to intertrochanteric fractures.
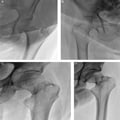
(Enlarge Image)Figure 1.
Garden classification. Type I and II (A and B) are considered "nondisplaced" and type III and IV (C and D) are "displaced" fractures.
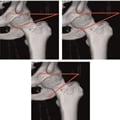
(Enlarge Image)Figure 2.
Pauwels classification based on the orientation of the fracture line in the femoral neck. Note increasing verticality of fracture line from type I to type III (A through C). (A) Type I<30 degrees. (B) Type II 30–50 degrees. (C) Type III>50 degrees.
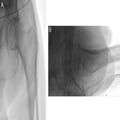
Femoral neck fracture that appears valgus impacted on anteroposterior view (A); however, it is seen to be displaced on lateral view (B).
FN fracture management and surgical treatment are based on a complex algorithm that includes fracture displacement, physiologic age of the patient, bone quality, and presence of an ipsilateral femoral shaft fracture. Early operative intervention has been shown to decrease the mortality risk and the risk of perioperative complications, such as pneumonia and pressure sores.[18] Nonoperative treatment of FN fractures rarely is indicated; it can be considered in non-ambulatory patients with minimal pain and in sick patients with excessive surgical risk; however, even in these instances the risks of nonoperative care over time may be greater than the risk of operative treatment. Operative treatment options include closed reduction percutaneous fixation (CRPF), open reduction internal fixation (ORIF), total hip arthroplasty (THA), and hemiarthroplasty (HA).
Nondisplaced FN fractures (including valgus impacted) commonly are treated with in situ fixation via CRPF using cancellous lag screws. In nondisplaced fracture patterns, the primary surgical goals are to provide stability, prevent fracture displacement, and allow for early mobilization.[19] CRPF with cancellous lag screws provides a stable construct, a minimally invasive approach, and decreased operative time. Typically, three cannulated cancellous screws are placed in an inverted triangle, with the inferior screw along the calcar on the posterior-inferior neck to prevent inferior fracture displacement. Operative pearls while performing CRPF include: ensuring the screw threads are past the fracture site to create a lag effect, maintaining a starting point at or above the level of the lesser trochanter to avoid a ST stress riser, and adding a washer for osteoporotic bone to decrease risk of screw penetration.[6,20]
In displaced fracture patterns in physiologically young patients, ORIF with a sliding hip screw (SHS) is frequently the treatment of choice. Adjunct fixation with an antirotation lag screw or a minifragment locking plate can be considered as well (Figure 4). In displaced fracture patterns, the primary treatment goal is anatomic reduction because malreduction has been shown to lead to poor clinical results, malunion, and increased reoperation rates.[21] If an attempt is made to close reduce a displaced FN fracture, the operating surgeon should have a low threshold for ORIF if an adequate reduction cannot be achieved with closed, indirect methods. SHS constructs are biomechanically superior to cannulated cancellous screws and are indicated in basicervical fractures or vertical fracture patterns (Pauwels 3) in a young patient.[22]

(Enlarge Image)Figure 4.
Displaced femoral neck fracture (A) treated with a fixed-angle sliding hip screw and antirotation screw (B).
In displaced fracture patterns in older individuals, hip arthroplasty is the primary treatment of choice because it allows early mobilization and return to function. The treatment decision for THA versus HA is based on the patient's activity level and the presence of preexisting hip osteoarthritis (OA). Older patients who are active and those with preexisting symptomatic hip OA are ideal candidates for THA. However, there is increased surgical morbidity and higher rates of dislocation with THA.[23] Older patients who are less active are generally well suited for HA. This highlights the multifaceted decision-making process in the treatment of all FN fractures. Optimal treatment involves a complex understanding of patient and fracture-specific characteristics, awareness of potential complications, and technical skill.
The FAITH (Fixation Alternatives in Treatment of Hip Fractures) trial published in 2017 compared 1079 patients ages 50 or older with both displaced and nondisplaced femoral neck fractures to either cancellous screw fixation versus SHS. This international multicenter trial showed no difference in outcomes in reoperation rate; however, basicervical neck fractures and more vertical fracture patterns trended towards better outcomes with sliding hip screw fixation, consistent with results of prior biomechanical studies.[24] A Cochrane review of over 6,000 patients also found no difference in outcomes between cancellous screws and SHS, although SHS fixation resulted in longer operative times and increased blood loss.[25] This systematic review, however, included 30 different trials of varying quality with heterogeneity in patient selection and inclusion of both displaced and nondisplaced fractures.
Recent observational studies have recommended expedited fixation of hip fractures to decrease associated morbidity and mortality;[18,26,27] however, no large standardized studies currently exist comparing early with delayed surgery. Some inherent bias may be present in these studies, however, as patients with increased acute comorbidities and risk are more often medically delayed from surgery and result in poorer outcomes. Currently, the newest American Academy of Orthopaedic Surgeons (AAOS) guidelines on elderly hip fractures state a moderate recommendation for surgery within 48 hr to improve outcome.[26] A large Canadian multicenter trial is currently in progress, which may further elucidate appropriate timing of surgery.[27]
Newer implant designs may increase stability of fixation and decrease collapse compared to current hardware. A dynamic locking plate (Targon Femoral Neck, B-Braun AG, Melsungen, Germany) with sliding partially threaded cancellous screws locked into a side plate on the proximal femur has shown lower rates of nonunion and collapse over other contemporary fixation devices in a recent British cohort study.[28] The theoretic benefit of this device is rotational advantage over SHS and axial load stability advantage over cancellous screws alone. In addition to new implants, modifications of existing implant use may provide improved biomechanical stability and functional outcomes for patients. In young patients with vertical fracture patterns, studies have shown the use of a medial buttress plate across the anterior inferior femoral neck in addition to cannulated screws or SHS may improve stability[29] and fracture union rates.[30,31]
Controversy still exists regarding hemiarthroplasty versus total hip arthroplasty in some elderly patients with displaced femoral neck fractures.[32] Quality outcomes studies are needed to determine cost efficacy, long-term outcomes, and overall impact on health systems.
In the choice of femoral stem fixation, practices are generally changing from cemented to uncemented press-fit stems.[6] Cemented stems offer more stability in severely osteoporotic bone and have been shown to have fewer reoperation rates than uncemented stems in a large Norwegian study.[33] However, the cemented group in this study had nearly 10 times the mortality risk as well as more than double the perioperative serious complication rate.[33] Recent studies have supported uncemented stems to reduce complications including embolization events, increased surgical time, and intraoperative blood loss.[34–36]
IT femoral fractures are extracapsular proximal femoral fractures located in the region between the greater and lesser trochanters. IT fractures represent approximately 50% of hip fractures in the elderly.[37] Like FN fractures, they occur with a bimodal distribution, with most caused by low-energy falls in the elderly.
The IT region represents the anatomic transition from the FN to the femoral shaft. It is made of dense cancellous bone, and it is highly vascularized by the medial and lateral femoral circumflex arteries, which provide an improved healing environment (in comparison to intracapsular FN fractures). The region includes the calcar femorale, which is a vertical wall of dense posteromedial bone that aids in force transfer from the FN to the femoral shaft.[38] Multiple muscle groups attach to the peritrochanteric region of the femur, which create fracture deforming forces that are critical in the understanding of fracture reduction.[12] These muscle forces and attachments are further discussed in the ST portion of this review.
Multiple IT fracture classification systems have been developed; however, there is none that is consistently used. The Evans classification divides IT fractures into type I, in which the primary fracture line extends proximally and laterally from the lesser trochanter, and type II, in which the fracture line extends distally and laterally.[39] The AO/OTA classification is a comprehensive system that defines IT fractures based on the number and orientation of fracture lines.[40] Most practicing surgeons define IT fractures based on stability. Stable IT fractures maintain an intact posteromedial cortex, and unstable fractures involve comminution of the posteromedial cortex.[41] Examples of unstable fracture patterns include fractures with a large posteromedial fragment, ST extension, and reverse obliquity fractures where the fracture line extends laterally and distally from the medial cortex.
Nonoperative management of IT femoral fractures is not indicated in the vast majority of individuals because of the high rate of associated morbidity and mortality. Nonoperative management results in prolonged immobilization and is associated with pneumonia, urinary tract infections, decubitus wounds, and deep venous thromboses.[38] Most IT fractures are treated operatively and should be completed within 48 hr of the injury unless additional medical optimization will significantly decrease the surgical risk.[42] Most IT fractures are managed with a sliding hip compression screw or a cephalomedullary nail (CMN); hip arthroplasty rarely is indicated in most centers. Fracture pattern dictates implant selection.
For stable IT fractures, SHS can be used. This involves a lateral plate with a fixed barrel through which a large compression screw enters the femoral head. The fracture is allowed to collapse in line with the angle of the barrel to provide dynamic interfragmentary compression and promote fracture healing.[38]
CMN can be effectively used in most IT fracture patterns and are the most effective in treating unstable fractures. The implant involves an intramedullary rod with a compression screw that inserts into the femoral head (Figure 5). It allows for dynamic compression of the fracture, but it also provides a biomechanical advantage as the nail acts as an intramedullary buttress preventing excessive shaft medialization[41] in addition to decreasing the lever arm of the construct. In the treatment of unstable IT fractures, the use of a CMN improved early mobility and decreased limb shortening when compared to the sliding hip screw.[43] Hip arthroplasty can provide positive functional results with early postoperative weightbearing for IT fractures with severe comminution, preexisting symptomatic osteoarthritis, or severely osteoporotic bone that would not hold internal fixation.[44] Optimal treatment of IT fractures requires intimate knowledge of IT anatomy, fracture patterns, and implant design.

(Enlarge Image)Figure 5.
Intertrochanteric femoral fracture (A) treated with a cephalomedullary nail (B).
For stable IT fractures, choice of implant has generally shown no significant difference in functional outcomes between SHS and intramedullary nailing,[45] despite some theoretical advantages. SHS have the benefit of being more cost effective but have a higher rate of femoral neck shortening[46] and medialization of the shaft,[47] which contribute to abductor dysfunction. Several studies suggest that this biomechanical advantage confers an improvement in early mobility,[43,46] but controls for preinjury function are needed to support this evidence.
The length of the IMN used has shown no difference in functional outcomes or periprosthetic fracture rate,[48,49] although costs and operative times are lower for short nails.[49] When periprosthetic fracture does occur, it happens at the midshaft in short nails and can often be fixed by exchanging for a long nail, whereas periprosthetic fracture in long nails tends to be a distal femoral fracture that can present greater treatment dilemmas. Distal locking results in decreased rates of periprosthetic fracture in both long and short nails.[49]
Although biomechanically advantageous in terms of cutout when compared with screw and sideplate implants,[50] helical blade intramedullary constructs confer no improvement in functional outcome or complications over single screw CMN fixation of the femoral head in IT fractures in some studies.[51,52] At least one study, however, shows an increased rate of medial blade penetration through the femoral head.[53] Furthermore, studies have shown better healing and functional recovery when using intramedullary constructs with dual screw head fixation.[54]
Studies show promising data regarding cement augmentation of IMN fixation in IT and ST fractures, and an augmented nail system has recently been approved in the US market for osteoporotic fractures. Cement augmentation has shown increased load to failure and stiffness over nonaugmented nails in cyclic testing,[55] and a recent prospective RCT showed more stability and less varus angulation with cement versus a metal device alone.[56]
Subtrochanteric (ST) fractures are defined as proximal femoral fractures occurring below the IT region and within 5 cm of the lesser trochanter of the femur. These fractures have a bimodal distribution occurring in young patients from high-energy trauma and in older patients from low-energy, osteoporotic mechanisms.[57] They also occur commonly in patients undergoing bisphosphonate therapy for osteoporosis.[58] ST fractures are challenging in reduction and fixation because the primarily flared cortical bone results in high rates of implant failure, nonunion, and malunion.[59–62]
The ST portion of the femur is composed of thick cortical bone in the normal and healthy physiologic state that does not fracture from low-energy mechanisms. Following Wolff's law of bone formation under mechanical stress, the medial side of this region withstands compressive forces of up 1,200 lb/in2 in a 200-lb male.[63] This high stress concentration has led to high rates of implant failures historically in ST fractures.
Understanding the deforming forces on a ST femoral fracture is crucial for reduction. The proximal fragment contains the lesser trochanter (LT) and greater trochanter (GT), which are the attachments for the iliopsoas (LT), short external rotators (GT), and gluteus minimus/medius (GT) muscles. These muscles displace the proximal fragment into flexion, external rotation, and abduction, respectively. The distal fragment contains the adductor tubercle and the linea aspera, which are the attachments for the adductor magnus and longus. These muscles will adduct the distal segment as well as shorten the deformed limb.
During reduction, care must be taken to avoid the medial circumflex artery that wraps around the LT as well as the sciatic nerve that runs posteromedial to the femur at this level.[12]
Classification systems for ST fractures are not commonly used. The Russell-Taylor classification can be used for diagnosis and prognosis; it is based on involvement of the LT and fracture extension into the piriformis fossa, which have implications for fracture fixation. Fracture patterns may vary from simple with good cortical contact to comminuted with bone loss.[64]
There are two main methods of fixation of ST fractures, intramedullary (IM) implants versus extramedullary implants. IM implants include antegrade statically locked nails, CMN and recon nails, while extramedullary implants include a fixed-angle blade plate or a proximal femoral locking plate.[65]
CMN provide the advantage of a more central longitudinal position (reduced lever arm) to counter bending forces from axial load.[66] IM nails also allow for immediate weight bearing as they are load-sharing constructs. Insertion of IM nails is a technique familiar to most orthopaedic surgeons, and the percutaneous technique allows for reduced blood loss, decreased operative time, and reduced hospital stay compared to open fixation with a blade plate.[67] Due to modern design advantages and increased efficiency of technique, IM nails have become the gold standard for treatment of most ST fractures. CMN with large lag screws are avoided in younger patients in order to prevent removal of a large portion of bone from the femoral neck. When fixation into the femoral head is necessary in younger patients with ST fractures, a recon nail with two smaller screws into the head is therefore preferred.
Fixed-angle plates allow for minimal bone removal and indirect reduction through the plate; however, they are technically challenging, do not allow for immediate weight bearing, and have a higher rate of complications. Forward et al.[68] demonstrated that CMN withstood greater load, more cycles of loading, and failed at a higher force than either proximal femoral locking plates or blade plates. When these constructs do fail, they invariably fail in varus malalignment.[59,69]
Reduction of ST femoral fractures may be performed closed; however, many require percutaneous or mini open adjunct techniques. The flexion and external rotation deformities must be corrected initially. Further reduction must be a stepwise approach with percutaneous approaches including clamps, Schanz pins, Cobb elevators, bone hooks, or ball spike pushers to maintain control of the short proximal segment (Figure 6).[70] Patient positioning can be either supine or lateral, and surgeon preference varies between a radiolucent flat table and fracture table. When treating ST fractures with an intramedullary device, close attention should be paid to ensure the starting point is not too far lateral to prevent varus malreduction.
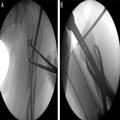
(Enlarge Image)Figure 6.
Percutaneous reduction maneuvers in a subtrochanteric femoral fracture using Schanz pin, bone hook, and reduction finger (A) and Schanz pin and clamp (B).
Postoperatively, the goal is early ambulation, as with most hip fractures, to prevent complications associated with prolonged bedrest. With fixed angle plating, relatively simple fracture patterns with good cortical contact and no trochanteric extension may be made weight bearing as tolerated immediately postoperatively, while unstable fractures should have protected weight bearing for several weeks. With a statically locked intramedullary device, weight bearing as tolerated can be allowed immediately postoperatively in these fractures. Union rates average around 10–12 wk, with longer periods for return to normal gait and prefracture level of activity.[71,72]
Comparison of trochanteric versus piriformis entry IMN for fixation of ST fractures have demonstrated no difference in blood loss, duration of surgery, intraoperative complications, union rate, or hip function scores.[73] A trochanteric entry nail has the potential disadvantage of increased morbidity to the abductor insertion in comparison to the piriformis entry but may have less risk of displacing fractures that propagate into the piriformis fossa.[74] Varus malalignment is theoretically less likely with a straight piriformis entry nail versus a curved nail; however, studies have shown no significant difference.[73]
Recent studies have suggested percutaneous cerclage wiring in conjunction with IMN to be an effective and safe reduction tool for fixation of ST fractures.[75–77] No increase in reoperation rate or implant-related failure was noted in these observational studies, but concern remains among some regarding the restriction of blood supply and callus formation at the fracture site with cerclage wires.[78] Blood flow studies and high-quality controlled studies could be helpful to test the efficacy and safety of this construct.
Hip fractures vary significantly in anatomy, pathogenesis, and treatment. Orthopaedic practitioners must be able to carefully distinguish between FN, IT, and ST femoral fractures. Diagnosis is essential in guiding treatment. The bimodal epidemiology should alert the practitioner to address important comorbid medical considerations, especially in elderly patients who have high levels of morbidity and mortality with these injuries. Care should be prompt, multidisciplinary, and integrated. If treated appropriately, good outcomes can be achieved for most hip fractures.

C/ San Pedro de Mezonzo nº 39-41
15701 – Santiago de Compostela
Teléfono: +34 986 417 374
Email: secretaria@sogacot.org
Coordinador del Portal y Responsable de Contenidos: Dr. Alejandro González- Carreró Sixto