Orthopedic foot/ankle surgery is a high risk specialty when it comes to malpractice claims. This study aims to evaluate the incidence, characteristics and outcome of claims in this area.
This was a retrospective, 10-year claim analysis, with data from an anonymous database. Baseline claim/claimant characteristics were collected from all orthopedic foot/ankle-related cases.
Of 460 claims in total, most were related to delay in/wrong diagnosis or to (complications of) elective surgical procedures. Whether a claim was settled was related to type of injury (fracture) and type of claim (diagnostic mistake). Median amount disbursed in settled claims was €12,549. Claim incidence did not increase over the years.
Missed fracture diagnosis and “failed”/disappointing results of elective surgical procedures were the most common causes for claims. Sufficient knowledge of missed (foot) fractures and clear communication/expectation management before elective procedures could help to improve quality of healthcare and patient satisfaction.
Recently, the fear of receiving a malpractice claim has increased and the consequences of that fear, such as overtreatment or depression/burnout among medical professionals, are not insignificant [1, 2]. The number of claims and the life time chance of receiving a claim may have increased over the years [3]. Orthopedic surgery has been defined as a high-risk specialty when it comes to the probability of receiving a claim [4, 5]. Within the orthopedic field, claims concerning the lower extremity seem to result in larger settlements then the upper extremity [6, 7]. Moreover, the foot and ankle region accounts for a large number of claims [8,9,10]. However, research on causality and risk factors for claims in this area is limited. Most studies focusing on claims in orthopedic surgery have investigated spinal surgery, or elective procedures such as joint replacements [11,12,13,14].
Identifying the most common reasons for claims in a specific field can lead to healthcare improvements to avoid patient damages and claims in the future. In the 90′s, MediRisk, one of the 2 medical liability insurance companies in the Netherlands, analyzed national claim data and found that most claims in the emergency department were related to misdiagnosis or treatment of fractures and tendon injuries [15]. Following these results, new guidelines and a safety net were installed, comprising, among other things, a daily radiology meeting where every X-ray of the day was discussed with both radiologist and supervisor. A study on hand and wrist injury-related malpractice claims evaluated the effect of that intervention and identified a mild decline in missed fractures [16].
This study aims to evaluate: 1. the incidence of claims related to orthopedic foot/ankle surgery, 2. the most common characteristics of claimants and claims, and 3. consequences and outcome of claims, in order to identify opportunities to improve care of foot/ankle conditions.
This is a retrospective, observational database study, investigating all claims related to foot/ankle injury within the scope of 10 years.
In the Netherlands, patients file a claim for compensation against the hospital and not directed at the physician personally, as is common in some other countries. MediRisk, as a medical liability insurer for its member hospitals, handles the claims of these patients on behalf of the hospitals. The burden of proof for medical negligence, damages and causation lies with the patient. When medical negligence has been established, MediRisk will compensate all reasonably damages caused by the negligence. At present over 95% of all cases are settled outside of court.
The data for this study were collected from the anonymous database of Medirisk. Medirisk is one of the 2 medical liability insurance companies in the Netherlands and represents around 50% of all non-academic hospitals in the country. The database is roughly classified for (among other things) concerned body part, cause, treating specialty, care process and consequences of claims, but also contains short descriptions of the individual claims (often in layman’s terms). All claims filed between 1–1–2007 and 12–31–2018 classified as concerning the “foot”, “ankle”, “toes” or “lower leg”, with the treating specialty being “surgery”, “orthopedic surgery”, “radiology” or “emergency medicine” were extracted. In addition to this, all claims with a description containing the words foot, ankle, toes or lower leg (and all medical and layman’s synonyms for those words) in combination with all terms suggesting injury or surgery were acquired from the database (full search in Appendix). Claims which were filed after 2016 (due to proportion of claims still open), not concerning the foot or ankle, not concerning orthopedic/trauma surgery and claims concerning patients younger than 18 years old were excluded.
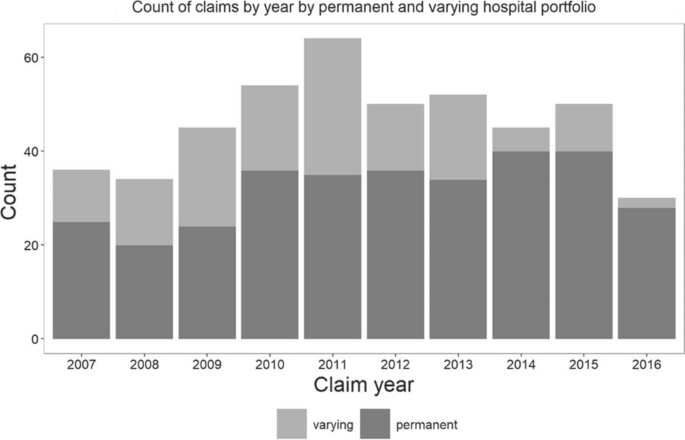
Extracted variables were (1) baseline characteristics such as age, gender and type of injury/affliction of the claimant, (2) treatment characteristics such as treating physician and operative treatment and (3) claim characteristics such as the type of claim (Table 1), consequences of the claim (both reported by claimant and medical expert), how the claim was handled (settled, declined, amicable settlement, closed without conclusion, negligible without harm) and what the costs were. These were displayed using descriptive statistics, reporting continuous variables in mean and standard deviation when normally distributed, in median and interquartile range when not normally distributed and categorical variables in numbers and percentages. Variables were compared between in- and excluded cases and between settled and declined claims using a Mann–Whitney U test for the continuous outcome measures and a Chi-Square for categorical outcome measures. Claim incidence was calculated per year corrected for the number of insured hospitals each year by separately depicting the constant group of hospitals (n = 42) and the number of hospitals that varied (n = 13).Table 1 Classification in types of claimsFull size table
Out of the 909 claims that were extracted from the database, 449 were excluded because they were filed after 2016 (n = 78), not concerning the foot or ankle (n = 305), not regarding a orthopedic/trauma-surgical problem (n = 15), the claimant was under 18 y/o (n = 43), or because there was not enough information to classify the claim properly (n = 8), leaving 460 for analysis. Excluded cases did not differ significantly from the included claims in age (47.1, SD 19.6 vs. 46.5 SD 15.9) or gender (218, 48.6% vs. 198, 43.0% males) of the claimant. There was a difference in location of the injury, which was significantly more in the lower leg for excluded cases, (193 vs 0, p < 0.01). The treating specialty was more often a general surgeon in excluded cases (246, 54.8% vs. 196, 42.6%) and excluded cases were more likely to be surgery related (242, 53.9% vs. 200, 43.5%) whereas included cases were more likely related to diagnosis. The status of excluded claims was more often still undecided (69, 15.4% vs. 23, 5.0%).
The overall number of claims varied slightly per year, with the largest number of settled claims in 2014. Regarding only the constant group of insured hospitals, the peak in claim incidence was in 2014/2015 with a subsequent decline in 2016 (Fig. 1).
Baseline characteristics of the claimant and the treatment he/she received are shown in Table 2. The claimant was 46.5 years old on average and female in 56.7%. The injury/affliction that was most frequently underlying the claim was a fracture and 80% of claims were related to either (the outcome/complications of) an operative procedure, or to a missed/wrong diagnosis (Fig. 2).Table 2 Baseline and surgical characteristics of claimantsFull size table
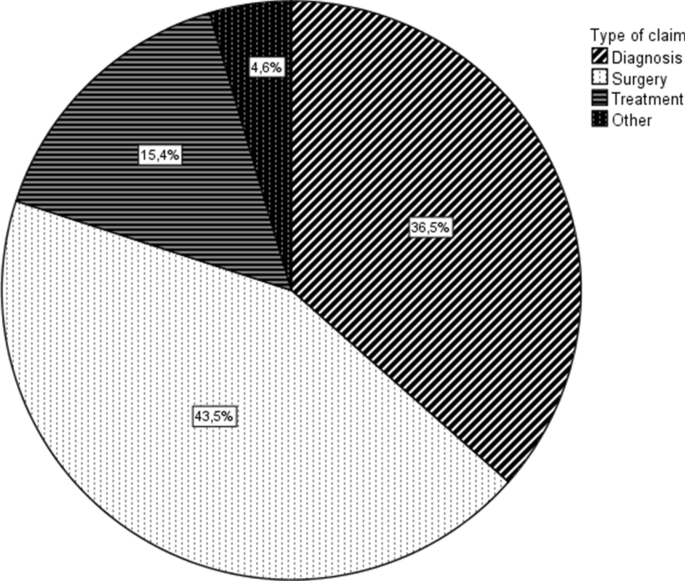
A subgroup analysis of only fracture-related claims showed that these were mostly fractures of the ankle (111, 53.4%) or the foot (85, 40.9%) and the type of claim was diagnostic in 106 cases, 51.0%. Surgical claims and treatment-related claims represented 23.6% (n = 49) and 22.1% (n = 46), respectively, in fractures. A subgroup analysis of all surgical claims showed that these were related to an elective procedure in 112 (56.0%) of cases. The underlying injury/affliction was missing in 49 (24.5%), but of the remaining cases it was a fracture in 49 (32.5%) and a hallux valgus in 46 (30.4%) cases. A larger proportion of female claimants (128, 64%) was seen in this subgroup compared to the entire study population. When specifically looking at diagnostic claims, these concerned fractures in 106 (63.1%), followed by tendon injuries in 22 (13.1%). The location of the injury was the foot in 86 (51.2%), the ankle in 64 (38.1%) and the toes in 18 (10.7%). Age and gender did not differ from the rest of the study population.
Out of 460 claims, 142 (30.9%) were settled/plaintiff verdict, 259 (56.3%) was declined/defense verdict and of the remainder; 36 (7.8%) came to an amicable settlement, 21 (4.6%) were closed without a conclusion and 2 (0.4%) were negligent without causing the claimant harm. Differences in baseline, surgical and claim characteristics between settled claims and declined claims are shown in Table 3. The median amount in euros disbursed in settled claims was €12,549 with a maximum of €322,149, IQR: [€4264–€36,145]. When analyzing the data per year, the year 2011 has the highest median disbursed amount (€23,566, IQR: €6,969–€69,689). Amicable settlements were worth €2641 on average (IQR: €1391–€7275). The most expensive claim of €325,000 concerned a 35 y/o male with a wrongly placed ankle prosthesis, which resulted in revision surgery and ultimately an amputation because of continuous pain. The second most expensive claim (€225,000) concerned a 45 y/o female with an intra-articular ankle fracture who did not receive a CT/MRI in the emergency department and initially received a cast instead of operative treatment, causing a delay in proper treatment and unresolved pain/limited function. The third most expensive claim (€190,000) concerned a Weber C ankle fracture in a 45 y/o male with limited functional outcome due to an operative procedure not performed according to protocol (ages and awarded amounts were rounded to guard privacy of claimant).Table 3 Baseline claim/claimant characteristics of settled and declined claimsFull size table
As shown in Table 4, the 3 most common patient-reported consequences were functional restriction, pain and revision surgery or readmission. When looking at the objective consequences (confirmed by a medical expert), the most common one is delay (in either treatment or diagnosis).Table 4 Claim consequences as reported by claimant and verified by medical expertFull size table
Events leading to filing a claim have a large impact on both the patient and the medical professionals involved [1]. Leaving patients unsatisfied goes directly against the fundamental motives of healthcare professionals to care for and cure patients. However, it is therefore especially important to evaluate the result of these good intentions. Analyzing claims gives us a unique chance to get a patient’s perspective on the quality of healthcare. Something that is particularly useful in a high-risk specialty such as foot/ankle surgery, with a large variety of pathology/injuries and a high rate of postoperative complications [17, 18]. This retrospective study therefore aimed to use foot/ankle surgery-related claims to identify opportunities to improve care of foot/ankle conditions.
The claim incidence did not seem to increase over the years. Although it is hard to draw conclusions because of the relatively small amount of claims per year in this subgroup, this seems comparable to literature. Klemann et al. have previously shown an increase in number of claims until 2012 and a stabilization after that in an investigation of all claims in the Netherlands from 2007 to 2016 [19]. A series of other studies could also not demonstrate an increase in the number of claims per year [4, 9]. However, there are also a few European studies that did find an increase in claim incidence [3, 7].
Considering the baseline characteristics of claimants, we found that claimants were on average young (46.5 y/o), female patients with a fracture. It has been previously reported that in general, elderly patients were less likely to file a claim [20]. In orthopedic surgery, this is supported by a Finnish study, linking all total hip and total knee replacements to the number of claims over a period of 5 years. They found that males and elderly patients were significantly less likely to file a claim, whereas increased comorbidity was positively associated with a claim [21]. However, a majority of male plaintiffs has also been described in a study looking at litigation after traumatic fractures [22]. Although we had no information about comorbidities, the claims in our cohort were mostly filed by young, female patients.
As for the reasons of filing a claim, in this cohort the claim was often related to a delay in/wrong diagnosis or to (complications of) an elective operative procedure. Both in general and in orthopedic surgery, multiple authors have previously suggested diagnostic mistakes as the most common cause for a claim [9, 23]. Injuries of the foot often have a large impact on functional recovery and, within the extremities, the highest number of missed fractures [24, 25], which could also explain the high percentage of foot injuries in our cohort, especially in the subgroup analyses of diagnostic claims. Even though ankle injuries are much more common, the percentage of foot and ankle claims in our cohort was comparable. Many studies have stressed the large impact of foot injuries on functional outcome and quality of life [26]. The chance of filing a claim also seems to correlate to the patient reported outcome, as illustrated by Thornes et al. who found that patients pursuing compensation had significantly worse outcome scores, unrelated to objective outcome measures and whether they were operatively or conservatively treated for their calcaneal fracture [27]. Calder et al. confirmed this in their cohort of Lisfranc injuries and also identified delay in diagnosis and treatment as important independent predicting factors in filing a claim [28].
The other major reason for filing a claim in this cohort, surgical errors or complaints about the outcome, have also been previously described [10, 29]. Casali et al. also found that claims were most often related to a surgery and that the majority of those procedures were elective [9]. Other authors have mentioned a misbalance in expectations before surgery and the result that follows [10, 30]. This could very well explain the fact that most surgical claims are related to an elective procedure, since in acute setting expectations might be lower [31].
Regarding the claim outcome, previous studies from the Netherlands have reported a settlement rate of 8–25% of claims [32,33,34]. This number was higher in our study (30.9%). An explanation might be that, in recent years, claims are more often filed by legal representatives. It is possible that through a selection process by these representatives, claims are only filed when there is a high probability of a settlement. This is supported by the mildly decreasing rate of declined claims over the past 10 years as Klemann et al. have shown in an investigation of all claims in the Netherlands from 2007 to 2016 [19].
In this cohort, settled claims were more often related to a fracture and to a missed/wrong diagnosis than declined claims. Bjørslev et al. previously analyzed claims after operative treatment of ankle fractures to identify iatrogenic risk factors for a settled/compensated claim. In contrast to our study, they found that most settled claims concerned a problem in the perioperative phase, most often incongruity of the ankle joint. However, they had a small cohort of 51 claims and did not analyze declined claims or foot injuries [35]. The average amount of €12,549 that was disbursed to patients in a plaintiff verdict was comparable to that of other studies from the Netherlands [19, 33, 34]. The patient-reported consequences (functional restriction, pain and revision surgery or readmission) are compatible with the earlier mentioned theory of a misbalance in expectations of surgery and the result that follows [10, 30]. One can theorize that claims may have been prevented by sufficient expectation management and informing patient of the risks, especially since the common objective consequences are not the same as the patients reported ones.
This study is subjected to a few limitations. First of all, the information supplied to the medical liability insurance company is from a patient perspective. Although it is checked and rated by medical professionals, the information extracted from the database is primarily “patient-reported”, making it subjective. Specific diagnoses were often not reported. Another possible limitation from this patient’s perspective is that it is not possible to directly link the highest awarded amounts to the biggest “mistakes”. Often, the awarded amount also depends on the consequences and circumstances of an individual claimant. However, to improve healthcare by identifying bottlenecks, the patient’s perspective on hospital procedures might even be more valuable than the objective events. Therefore, the patient’s perspective is at the same time a major strength of this study, since patient’s satisfaction plays a big part in quality of care.
The second limitation is that, because of the patient-reported data, this study could not give a specialist perspective. It might have been valuable to identify how many claims a certain medical professional receives and what the risk factors for receiving a claim are. However, this is out of scope of the current trial and has been previously studied [9].
Finally, although it is important to compare results of this study with those of others, not all aspects can be compared between countries. Because of widely varying juridical claim procedures, information such as the rate of settled/declined claims and awarded amounts for settled claims, cannot be compared. Therefore, we were limited to a small number of previous cohorts from the Netherlands for these comparisons.
Despite the limitations, we feel that this study provides valuable information for the orthopedic/ trauma surgical community. Although claims have been previously studied in orthopedic fracture surgery, this study represents the largest cohort that focuses on foot/ankle surgery [22, 35]. Given the high complication rate in this area of orthopedic surgery, it is important to identify pitfalls in (operative) care and communication, not only to prevent malpractice claims, but to improve the quality of care. In conclusion, the results of this study show that missed (foot) fractures and “failed”/disappointing results of elective operative procedures are the most common causes for claims. Although not all (alleged) medical errors can be avoided, some lessons can be learned from this conclusion. First of all, a high index of suspicion and adequate knowledge of the most commonly missed foot fractures could decrease the number of missed/wrong diagnoses in the acute setting and benefit timely and adequate treatment. Secondly, the importance of clear communication/expectation management before elective procedures is once more underlined.
The anonymous database is available upon request.
N/A.
No funding was used for this research.
TS conceived of the idea; FS, PW, OD and TS designed the study; PW and OD provided the data and assisted FS in data analysis, FS drafted the manuscript, GK and TS aided in interpreting the results. All authors critically revised the manuscript.
Correspondence to Fay R. K. Sanders or Tim Schepers.
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Since this study was performed using data from an anonymized database, patient’s informed consent or ethical committee approval was not required.
N/A, anonymous data.
N/A.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this l