Recurrent lumbar disc herniation (LDH) is the most frequent reason for reoperation after lumbar microdiscectomy. While several risk factors for recurrent LDH have been well-described, the effect of age on recurrence remains unclear, especially concerning the timing of recurrent LDH.
From a prospective registry, we identified all patients who underwent tubular microdiscectomy for LDH. Recurrent LDH was defined as reoperation for LDH at the same index level and side. The associations among age and incidence of recurrent LDH as well as on time to recurrent LDH were statistically evaluated using multivariable analysis of covariance, linear regression, and Cox proportional hazards modelling.
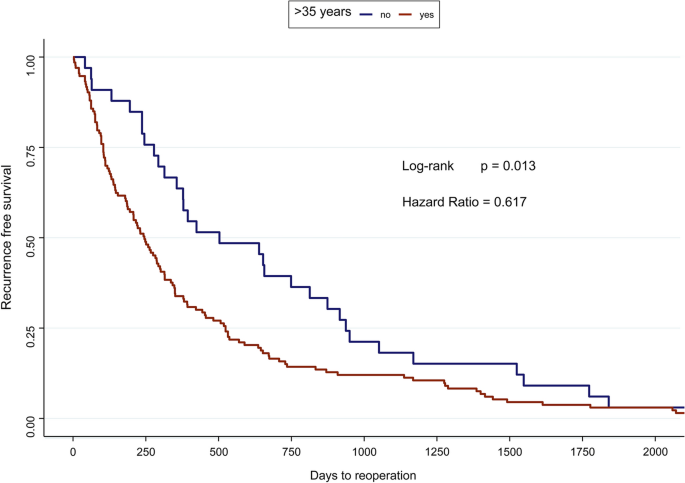
Of the 3013 patients who underwent surgery for LDH, 166 (5.5%) had to undergo reoperation due to LDH recurrence. Uni- and multivariable analysis revealed no influence of age on the incidence of recurrent LDH (both p > 0.05). Linear regression indicated earlier reoperation in older patients, both with (β = −0.248) and without (β = −0.374) correction for confounders (both p < 0.05). An additional survival analysis found that patients aged over 35 years had recurrent LDH significantly earlier (hazard ratio 0.617, p = 0.013).
In an analysis of a large prospective database of patients undergoing microdiscectomy for lumbar disc herniation, we found that younger patients do not have a higher reoperation probability than their older counterparts, even after correcting for multiple confounders. However, older patients tend to experience recurrent LDH significantly earlier after the index surgery compared to younger patients.
Lumbar disc herniation (LDH) is one of the most common indications for lumbar spine surgery [1]. Although minimally invasive surgical techniques are becoming more and more common in lumbar neurosurgery, the current literature suggests that 3 to 13% of all patients undergo redo surgery because of a LDH recurrence [2,3,4,5,6].
As a result, it is important for both physicians and patients to identify risk factors for LDH recurrence, so that optimized individual pre- and postoperative patient management may lead to a lower occurrence. There are many studies that have identified several risk factors, however not without controversial results [5,6,7,8,9,10,11]. While certain risk factors, e.g. active smoking status, have been demonstrated to contribute to a higher probability of LDH recurrence, there are many other risk factors like age or gender which have more subtle effect on LDH recurrence, and which have thus demonstrated inconsistent results in multiple studies.
This study is a result of a clinical hypothesis generated by the surgeon’s observation that LDH recurrence is more common in younger patients, but that LDH recurrence occurs significantly earlier in older patients compared to their younger counterparts. The first part of this hypothesis is also further corroborated by a review conducted by Hlubek et Mundis in 2017 [6], in which younger age is stated as risk factor for LDH recurrence. On the other hand however, many other studies suggest an absent [5, 7, 9,10,11] or even a reversed [12] effect of age on LDH recurrence.
Furthermore, to the best knowledge of the authors, there is currently no study investigating the effect of age on time to recurrence. Better comprehension of this phenomenon may also contribute to a better understanding of the risk factors and mechanisms contributing to LDH recurrence.
The aim of this study is to describe patient profiles of patients undergoing reoperation due to LDH recurrence, and especially to compare the age of the reoperated patients to the patient subgroup without reoperation. Additionally, we aim to describe the association of age and time to reoperation for recurrent LDH.
Out of a prospective institutional registry of lumbar surgical interventions, all patients who underwent first time tubular microdiscectomy (tMD) for lumbar disc herniation were identified. All patients were operated between December 2010 and November 2019 by one senior neurosurgeon (M.L.S.) at a specialized spine centre. Indications for surgery and surgical technique are laid out in extenso in previous publications.[13,14,15] Patients aged > 80 or with a body mass index (BMI) > 35 or American Society of Anesthesiologists (ASA) score > 2 were not eligible to undergo surgery in such a setting due to local insurance regulation restrictions.
This institutional registry was approved by the local institutional review board (Medical Research Ethics Committees United, Registration Number: W16.065), and this study was performed according to the Declaration of Helsinki. All individual patients in this study provided written informed consent.
LDH recurrence was defined as reoperation for recurrent LDH at the same index and the same side. For all patients included in this study, any recurrence of LDH up to this study was tracked and noted, as well as the time from surgery to reoperation. Patients were systematically categorized into two groups, one with an LDH reoperation and one without any. Patients completed a standardized questionnaire containing a numeric rating scale (NRS) for back pain and leg pain severity, as well as a validated Dutch version of the Oswestry Disability Index (ODI) as a measure of functional disability. After 12 and 24 months after surgical intervention, follow-up questionnaires containing the same PROMs were automatically sent to the patients via e-mail.[16]
Continuous data are given as mean ± standard deviation, and categorical data as numbers (percentages). For determining intergroup differences in age, we conducted a Student’s t test. Additionally, we performed analysis of covariance (ANCOVA) with age as dependent value and LDH recurrence, gender, smoking status, and BMI as independent values. In a more extensive multivariable analysis, we further added baseline PROM values to the independent values in a second ANCOVA model.
For the analysis of time to recurrence, we conducted a linear regression analysis for determining any correlation between age and time to recurrence, also adjusting for the abovementioned covariated in a multivariable analysis. We additionally performed a survival analysis using a Cox proportional hazards model for time to recurrence, comparing patients aged 35 years or younger with those aged over 35 years. A log-rank test was applied to test for significance. For all analyses, a 2-tailed p ≤ 0.05 was considered as statistically significant. All analyses were carried out using R version 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria).
The patient flow throughout this analysis is shown in Figure 1. Overall, data from 4755 patients were available, of which 3012 (63.3%) underwent tMD for LDH. All these patients had complete clinical, pre- and intra-operative data, as well as complete age records and a follow-up of at least 12 months. Out of these patients, 166 (5.5%) had reoperation for LDH recurrence, 7 (0.2%) within the first month and 16 (0.5%) within the first two months. Mean time from surgery to reoperation was 476 ± 525 days. Other baseline values are shown in Table 1.
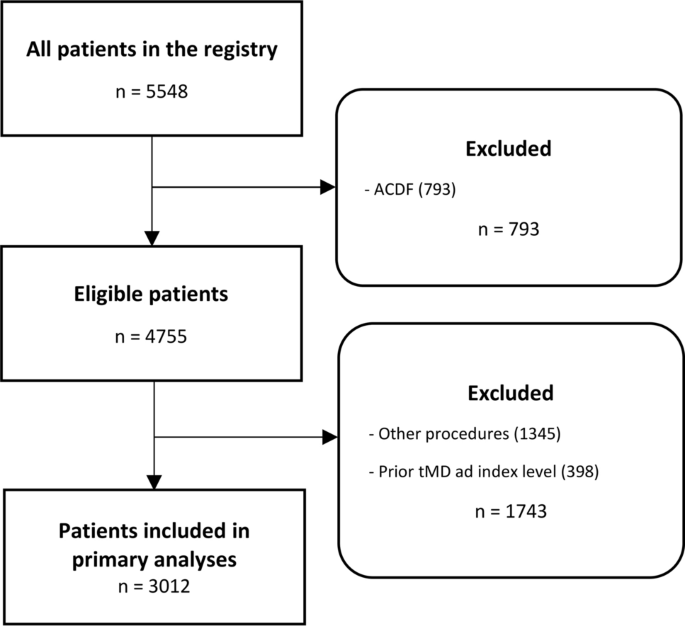
Table 1 Baseline patient characteristicsFull size table
Between patients who underwent reoperation for LDH recurrence (mean age: 46 ± 12 years) and those who did not (mean age: 45 ± 13), no statistically significant age difference could be stated (p = 0.85). The graphical illustration is shown in Figure 2. The results of the multivariable ANCOVA are shown in Table 2. In summary, our analysis did not show any correlation between LDH recurrence and Age (F = 0.757, p = 0.384). When additionally adding PROM baseline values to the ANCOVA, as shown in Table 3, similar results were obtained (p = 0.996).
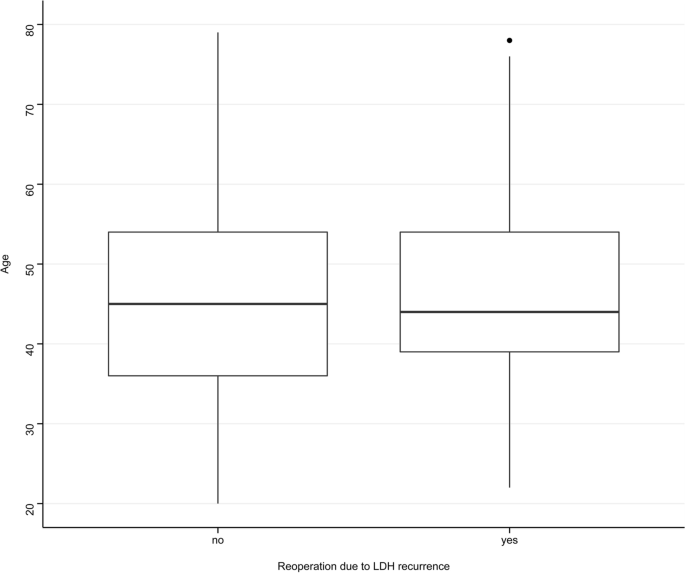
Table 2 ANCOVA analysis of the influence of age (dependent variable) on recurrent LDH while controlling for other potential confounding variablesFull size tableTable 3 ANCOVA analysis of the influence of age (dependent variable) on recurrent LDH while controlling for other potential confounding variables as well as baseline PROMsFull size table
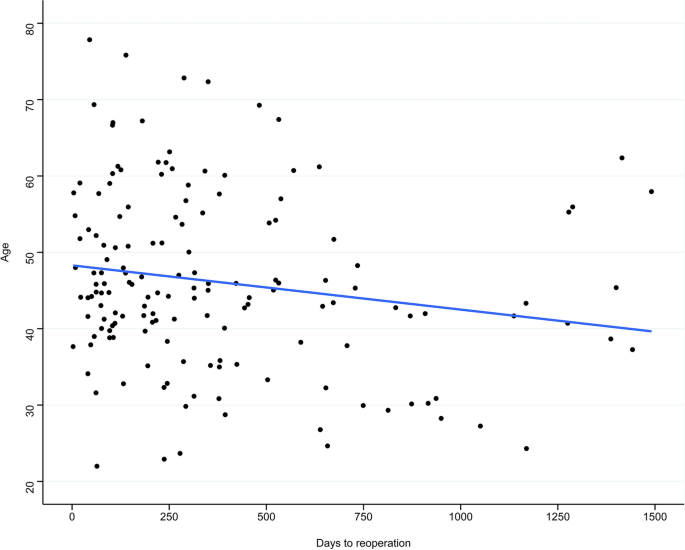
The linear regression model is shown in Figure 3. Our analysis showed a statistically significant correlation between age and time to reoperation, however with a high variability (β = −0.248, R2 = 0.06, p = 0.001). After adjusting for gender, smoking status, and BMI, a higher R2 value is obtained while preserving statistical significance (β = −0.374, R2 = 0.22, p = 0.008). The Cox proportional hazards model also indicated earlier recurrence requiring surgery in older patients aged over 35 (hazard ratio = 0.617, p = 0.013), as illustrated in Figure 3.
A registry of prospectively collected data of 3013 patient that underwent tMD for LDH was retrospectively analysed. Out of these, 166 (5.5%) underwent reoperation due to LDH recurrence. We compared patients who underwent reoperation for LDH to those who did not, with no difference in age even after controlling for multiple potential confounders. Furthermore, linear regression analysis suggested a shorter time to reoperation for recurrent LDH in patients aged over 35 years compared to their younger counterparts, however with a wide range of variability. This was subsequently robustly validated in a survival analysis with the same result, Fig. 4
Our data showed an LDH recurrence reoperation rate of 5.5%. This value compares favourably with the literature, which describes different values ranging from 3 to 13% [2,3,4,5,6]. We have previously analysed the effect of surgeon experience with rates of recurrent LDH [15]. Our initial clinical hypothesis stated that younger patients tend to suffer from LDH recurrence more frequently, and therefore hypothetically must undergo reoperation more frequently. A meta-analysis conducted by Hlubek et Mundis [6] and a recent analysis from the Spine Patients Outcomes Research Trial (SPORT) in 2017 [17] has indeed defined younger patients without neurological deficits as those at highest risk for LDH recurrence. One possible explanation for these literature findings is that approximately one third of all LDH recurrences are a consequence of a traumatic event [18], and therefore may occur more often in the younger and more active population.
However, our data did not show any effect of age on LDH recurrence, which compares well to most other studies—disregarding the two studies mentioned above—investigating risk factors for LDH recurrence [5, 7, 9,10,11]. While on the one hand, traumatic events are a possible aetiology, true degenerative disc disease is more common in older patients, which has been previously associated with more frequent re-herniations [18, 19]. These two different potential aetiologies may balance each other out in a diverse patient population, and therefore may explain the overall absent effect of age on LDH recurrence.
The timing of recurrence after lumbar discectomy is—to the author’s best knowledge—an as of yet unresearched topic in the literature. There are several studies investigating risk factors for LDH recurrence, but none investigating their effect of its development velocity. Our study investigated the effect of age on time to reoperation, and our data suggest that older patients tend to undergo reoperation significantly earlier than their younger counterparts.
One possible explanation might be the different aetiologies as explained above, with a higher incidence of traumatic events in the younger cohort [17] and true degenerative disc disease in the older population [18, 19]. However, it is crucial to point out that while the results concerning time to reoperation reached statistical significance, they also showed broad variability with vastly different interpersonal results even after correcting for multiple potential confounders.
Our study is firstly limited by its retrospective nature. All data were collected prospectively and all patients with sufficient data were included. All complications and reoperations were captured systematically. Additionally, a possible centre bias cannot be excluded, as all data stems from a single centre and a single neurosurgeon. Because local insurance regulations did not allow high-risk patients to be operated on—thus those with a BMI > 33, ASA Score of 3 or greater, and age over 80 years—further bias may have been introduced.
In an analysis of a large prospective database of patients undergoing microdiscectomy for lumbar disc herniation, we found that younger patients do not have a higher reoperation probability than their older counterparts, even after correcting for multiple confounders. However, older patients tend to experience recurrent LDH significantly earlier after the index surgery compared to younger patients.
Open Access funding provided by University of Zurich. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Correspondence to Victor E. Staartjes.
The authors declare that the article and its content were composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence